Treatment for NLPHL in abdomen only
Comments
-
Hope !Iluvlucy said:Not the type of support I need but thanks anyway
Suck it up and adapt is not much support. Will look for a bit softer approach elsewhere. I also didn't see my post as whining but you are entitled to your interpretation. Have a good day.
P
Please do not leave this Board, iluv....
I'm sorry that our previous discussions regarding NLPHL seems to be gone, but most of the stuff above on this thread is directly relevant to you. PM or post here for any restatement that you may need, or any questions of any form.
It is pretty outrageous that they have you down as Classical (CHl). But as I have noted, it tends to be treated as-such anyway. It may be that your records show that the TREATMENT protocol is per Classical, not the diagnosis. Just a possibility.
R-CHOP is what most clinics administer for your disease and stage, that or R-ABVD. Be certain that they ARE giving yuo the Rituxan, since CHl does NOT express the CD-20 cell, but NHLHL DOES. Rituxan has strong proven success is lessing relapse vs. CHOP alone for NLPHL.
I would demand a consult with your doctor, a face-to-face, and demand that this all be cleared up. It is egregious enough to use the "L" word if he hee-haws and avoids the discussion.
It is correct however that Stage III lymphoma of any form requires full application chemo, and I don't know of any other drug combinations commonly used first-line for indolent lymphomas.
I hope to hear from you soon,
max
0 -
Thanks, MaxHope !
Please do not leave this Board, iluv....
I'm sorry that our previous discussions regarding NLPHL seems to be gone, but most of the stuff above on this thread is directly relevant to you. PM or post here for any restatement that you may need, or any questions of any form.
It is pretty outrageous that they have you down as Classical (CHl). But as I have noted, it tends to be treated as-such anyway. It may be that your records show that the TREATMENT protocol is per Classical, not the diagnosis. Just a possibility.
R-CHOP is what most clinics administer for your disease and stage, that or R-ABVD. Be certain that they ARE giving yuo the Rituxan, since CHl does NOT express the CD-20 cell, but NHLHL DOES. Rituxan has strong proven success is lessing relapse vs. CHOP alone for NLPHL.
I would demand a consult with your doctor, a face-to-face, and demand that this all be cleared up. It is egregious enough to use the "L" word if he hee-haws and avoids the discussion.
It is correct however that Stage III lymphoma of any form requires full application chemo, and I don't know of any other drug combinations commonly used first-line for indolent lymphomas.
I hope to hear from you soon,
max
Thanks, Max. The only reason I want 2 other opinions is that I have read of many protocols to treat Stage IIIA NPLHL and some non traditional approaches. I understand the intricacies of the subtype. I have done incredible research and know that there is more to offer than R-CHOP or R-ABVD. I want to have the discussion with someone on the cusp of the research. I know that I probably will end up just where I started but don't want regrets of not exploring them first. In the meantime, I'm going through all the stages of grieving in a roller coaster fashion and dragging my poor hubby along for the ride. He says he never knows what he will find from moment to moment. He such a dear man!
P
0 -
Sorry you think me harsh.
Life can be harsh. Sometimes we just have to face reality. However please don’t leave the board because of me. I will say no more. And if you find an easy, no pain, no suffering , not inconvenient, risk-free cure for lymphoma that lets us keep our hair please share it. I am convinced there will eventually be one. Seriously - best of luck. I wish you well.
0 -
Eh....Iluvlucy said:Thanks, Max
Thanks, Max. The only reason I want 2 other opinions is that I have read of many protocols to treat Stage IIIA NPLHL and some non traditional approaches. I understand the intricacies of the subtype. I have done incredible research and know that there is more to offer than R-CHOP or R-ABVD. I want to have the discussion with someone on the cusp of the research. I know that I probably will end up just where I started but don't want regrets of not exploring them first. In the meantime, I'm going through all the stages of grieving in a roller coaster fashion and dragging my poor hubby along for the ride. He says he never knows what he will find from moment to moment. He such a dear man!
P
P,
I say the same thing about my wife, and she is not sick !
0 -
Luck of the drawIluvlucy said:Thanks, Max
Thanks, Max. The only reason I want 2 other opinions is that I have read of many protocols to treat Stage IIIA NPLHL and some non traditional approaches. I understand the intricacies of the subtype. I have done incredible research and know that there is more to offer than R-CHOP or R-ABVD. I want to have the discussion with someone on the cusp of the research. I know that I probably will end up just where I started but don't want regrets of not exploring them first. In the meantime, I'm going through all the stages of grieving in a roller coaster fashion and dragging my poor hubby along for the ride. He says he never knows what he will find from moment to moment. He such a dear man!
P
P,
Like Po, I was first diagnosed with cancer in 2009 -- but with the NLPHL. Massively covered with tumors, as I've described before. Technically Stage III since there was no bone marrow involvement, but with a lot more disease than most Stage IV patients present with.
I was then 53, but my hematologist, who is world-class, used statistics for me for a 60 year-old, a threshold when surival statistics change substantially for most strains of lymphoma. He told my wife and I that I had a 60% chance of living 5 years, but he said he felt pretty confident. My take of that (perhaps odd), was "Wow ! Those are good odds !" I had previously done research on the numbers, and had compiled the exact same probabilities before he spoke with us. Ten years later, I am still N.E.D.
Some cancers, like many forms of brain, have a 1% to 5% survivorship (recall John McCain, Joe Biden's son, and Teddy Kennedy). Pancreatic late-stage is not good. Same for lung or colorectal. Same for Peritoneal, ovarian, and many others. Prostate Stage IV is by definition terminal, but moves very slowly in most treatment cases. (I've had Stage II Prostate, but am apparantly cancer-free today.) I am not saying that there is anything good about lymphoma, but from a purely rational/logical analysis, it is way better than some other possibilities. Some personalities will take solace in that, some will not. Neither reaction is wrong. The human animal is not just logic and statistics -- a good thing.
People always ask me, "How did cancer change you ?" I give them an unexpected reply: "It made me more intensly like I had always been." Although it is a terrible development, most people deal with having cancer the same way they deal with anything else. Religious people remain religious, secualrists remain secular. Optimists remain optimistic, pessimists become more so. Obsessive types continue to obsess; free spirits worry only a little.
A dear friend died of prostate about six years ago. Because his relatives were all out of state, I drove him to almost all appointments during his last year till he went in to hospice. He had had PCa 12 years at that time. We were discussing a mild stroke he had suffered about five years earlier. I asked him what he thought and felt before he passed out from the stroke (he had been at home alone when it occured), and he said he remembered thinking that it was in a fact a stroke, and he recalled thinking in response, "Well, if I don't wake up, it's been a good run....no regrets."
His time during the last year with cancer was the same; his attitude was always, "If this is it, let's get it on." He always told people to feel no sorrow, that he was good with everything in his life.
His story is peculiar and not the norm. His attitude is very unlike my own even. The point is that we all bring our own views and attitudes to this disease. Use your skills as only you know them. But do take care of your emotional situation with the tools you possess, and possessed a year ago, before diagnosis. Because very likely, you will get through this relatively quickly, and have many decades of heath before you.
max
0 -
Look to others for examples
In 2008, we hoped that I had Hodgkin's. Didn't. Just to show the advancements that are being made, my prognosis, when one even applied, was poor. It immediately dropped to extremely poor. This was in 2009. Since then, there was no patient group for me to belong to. It was only a matter of if I survived or not. In 2015, I had two different aggressive T-Cell non-Hodgkin's lymphomas as well as the AML precursor MDS in my marrow at 26%. In 2017, I was given a 99.5% chance of not making it. Greater understanding of NLPHL has lead the way to greeater success. No time to panic - rather time to live and enjoy life. Every day in the US, 102 people die suddenly in traffic accidents. No warning, no recovery. Those of us with cancer are a universe ahead of them.
As to dealing with the diagnosis, what do you believe? Those with a strong philosophy, world view, beleief system or religion report a far easier time dealing with it all. There is an article addressing this in the 2018 bonue issue of CURE magazine. EDIT: Find the CURE Magazine story here.
0 -
I just got diagnosed with NLPHL also
Hi,
I am located in Toronto, Canada and came across this forum over the weekend while researching about NLPHL treatment options. I am a 26 year old male and was diagnosed last week with early stage NLPHL. I do not smoke, have a glass of wine a few times a year, do triathlons, play soccer and eat pretty well. My extended family (uncle, garndparents etc) have some history with lung cancer and heart disease but not my parents. It's not that easy to find primary sources online with people dealing with NLPHL, that's why I was happy to see this forum thread and want to explain my situation in case it can be of any help to someone in the present/future. I also have a few questions at the end regarding treatment options.
My diagnosis process up to now- I noticed a lump in my neck (feels like a golf ball inside my neck) while massaging my neck one day in early November 2018
- I got it checked out at a hospital and had an ultrasound done
- Ultrasound located the mass on my left neck and the doctor told me its likely a swollen lymph node
- I told the doctors I had no colds or sicknesses for months leading up to the day I noticed the lump
- Was referred to a throat specialist at the hospital who also couldn't figure out why I had a swollen lymph node if I hadn't been sick for a long time
- Was referred to an oncologist at Toronto General Hospital who said I may have a branchial cleft cyst and was ordered a head/neck CT scan
- CT scan showed a 4cm oval mass suggestive of either lymphadenopathy or a benign peripheral nerve sheath tumor (schwannoma)
- Ultrasound guided fine needle aspiration biopsy was ordered to narrow down the diagnosis.
- The biopsy involved 2 core (solid) samples and 3 liquid samples.
- Pathology report on the biopsy was suspicious for Hodgkin lymphoma because malignant cells were found and some cells that were observed resembled Reed Sternberg cells
- I was referred to a lymphoma doctor at Princess Margaret Hospital in Toronto and my oncologist ordered a thorax, abdomen and pelvis CT scan to check if there are any other swollen lymph nodes in my body.
- Oncologist also ordered a surgical biopsy because the 1st biopsy didn't retrieve large enough samples to locate/pinpoint the Reed Sternberg cells as there was still a chance I could have non-hodgkin's
- Lymphoma doctor ordered a PET scan
- Thorax, abdomen and pelvis CT scan revealed no evidence of swollen nodes or tumors located anywhere else except for the one in my neck.
- PET scan reveled cancerous cell activity in the lump in my neck and some activity in the area around the lump as well as some activity on the other side of my neck (i feel no lumps there)
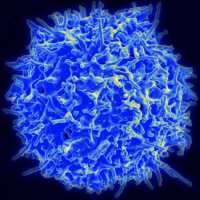
- Surgical biopsy done and pathology report diagnosis concluded I have Nodular Lymphocyte Predominant Hodgkin Lymphoma. Numerous small CD3+ T-cells and CD20+ B cells were found
- Was told last week I have early stage NLPHL and I am closer to a stage 2A because of some activity on the other side of my neck. I have no B symptoms (no night sweats, fevers, excessive weight loss etc.) The only physical symptom I have is the painless lump in my neck and this remained the only symptom from the 1st day I noticed the lump till now.
- Lymphoma doctor is recommending 2 cycles of ABVD, 1 month break followed by radiation therapy. This proposed treatment plan is being presented to the lymphoma board at Princess Margaret today where all the lymphoma doctors gather to discuss the best treatment plan in a collaborative effort.
Reading all the threads above especially Max's posts revealed to me (along with some digging on google) that Rituximab is a popular drug of choice to treat NLPHL. I brought this up to my lymphoma doctor and found out that this drug is not covered by my province's (Ontario) health care program. Its cost is covered for certain specific lymphoma diagnosis but not for NLPHL. Regardless, I've asked my lymphoma doctor to bring up the possibility of using Rituximab (I would have to pay) for my treatment when my case/proposed treatment plan is discussed at the lymphoma board meeting.
A few questions:- Has anyone had any experiences being treated for early stage NLPHL with ABVD and radiation only with no rituximab? I ask this because R-ABVD seems common in posts above
- In doing some research online surgical removal is sometimes recommended for early stage NLPHL but was told due to the size of my lump and cancerous cell activity being located around the lump and on the other side of my neck that surgical removal is not recommended. Chemo+ radiation is more effective. Has anyone had NLPHL treated with surgery alone?
- Can ABVD alone treat NLPHL if scans are done after chemo treatment and show no signs of cancerous activity or is radiation always required after chemo?
I am just worried about all the treatment plans out there because I've been reading so many different combinations online. I trust the doctors at Princes Margaret which is well known for their cancer research and treatment but I know there isn't a golden standard for NLPHL because it is a very unique and rare type of Lymphoma with very little studies done. I just don't want to subject my body to anything I don't need to (Iam sure everyone going through cancer thinks the same things) especially if some of these chemo drugs may cause long term permanent side effects like lung problems from using the Belomycin drug in ABVD.
Thank you for your time to read my post. Hopefully me explaining the process I went through up to now to get a diagnosis will help anyone in the future dealing with Hodgkin's/NLPHL. Any insight into the questions above would be greatly appreciated
 0
0 - I noticed a lump in my neck (feels like a golf ball inside my neck) while massaging my neck one day in early November 2018
-
Welcome
Welcome to you, iam.
You've scanned the posts above in this tread, but it might be useful for you to do so again.
Yes, ABVD without Rituxan was the standard therapy for NLPHL for many years, prior to the development of Rituxan. It has a record of being very effective. Adding the rituxan helps statistically. Prior to ABVD, MOPP was the standard Hodgkin's treatment, and MOPP is still in rare use today.
Rituxan is not used with any form of HL even in the US, exept for NLPHL, because Rituxan kills the CD-20 cell, and NLPHL is the only form of HL that presents with CD-20. Oncologists so seldom see NLPHL that they may be unaware of the benefit of Rituxan against it. I would guess that 2 cycles of ABVD with follow-on radiation would be totally effective. But, if you choose to pay to add Rituxan yourself, it certainly can't hurt.
You mention your diet and health overall. No one knows what causes lymphoma, and it is not linked (in any convincing manner) with much of anything, so know that you are not to blame for this.
max
0 -
I agree with Max
I had 3 opinions for my Stage IIIA NLPHL diagnosed a few months ago. Although I did have 3 somewhat different opinions they ALL included Rituxan. I had my first chemo a week ago. Had R-CHOP ( rituxan, cytoxan, adriamycin, vincristine, and prednisone. My case was reviewed in 3 different tumor boards as well. 2 local tumor boards and one national as well. What Im reading is that the latest theory is to avoid over treatment as this is a slow growing lymphoma and you are quite young. Although I wouldn't consider myself old, I am far older than you and they still wanted to avoid over treatment. I dont know the answer about radiation, but when initially they thought I had StageIA, they were recommending involved site radiation only, meaning just radiating my armpit where the lymphnodes were located. I, too, do not have a family history or lifestyle that would put me at high risk. I am participating in a BIO bank at The University of Chicago Cancer Center so that they can do ongoing research and gather lifestyle and med history info on me so hopefully they can find out more about this cancer and hiw to prevent it. Good luck to you and my best wishes.
Paula
0 -
Rituxan reactions?
I am being treated with Rituxan for relapsed NLPHL. Currently in maintenance stage with the Rituxan and seemingly having issues for the first time -- after a year of Rituxan infusions with no negative reactions -- with itching and general feelings of malaise and sickness. PET/CT was ordered off-schedule b/c of my symptoms and it showed moderate increase FDG activity in two nodes (4.6 SUV). Doc said he is not worried b/c SUV is not high enough to indicate serious metabolic activity in the nodes. However, the symptoms continue and doc does not necessarily think they are Rituxan related.
I have had a thousand tests to rule out infections, antibody reactions, viruses, etc. and nothing shows up. Have been on Predisone twice and now on Gabapentin. No effect on symptoms. Has anyone had similar reactions to Rituxan? If this NLPHL board is not right place to ask, can you recommend a better one? Maybe follicular lymphoma patient board... Thanks.
0 -
Symptoms
Tgy,
I am convinced that side-effects, in most cases, simply cannot be authoratatively linked to any cause. There may be "best guesses', but seldom certitude. Say a person were to go on just the drug Prednisone, and got agitated and gained fluid weight: that would be a slam dunk -- the Prednisone was the cause. But very few cases are so clear-cut. And most people here are on a collection of chemo drugs and others, and many have the SAME side-effects, and some side-effects occure soon, while others are know to delay for years at times (such as Adriamycine [Rubex] causing heart muscle thickening). So you might never know.
I have been N.E.D. for ten years now from NLPHL, and was never on maintenance. Yet, the last two years, I have had terrible....itching ! Go figure. The N.P. has suggested everything from hot showers to this-or-that as the cause. She is not worried about relapse, and has ordered no scans. I get an annual CBC, metabolic profile, and touch exam, and none indicate any problems.
Many lymphomas take JUST Rituxan for maintenance, and it is a "disease-wide issue, so there is no right or wrong thread to be on. This is fine, or start another -- they are free. I am thankful you have been in C.R. and that the PET shows no real cause for concern. It seems your doctor is following due diligence and watching this with an appropriate level of aggressiveness. He or she, most likely, like us, will never know what caused the itching. But the "other" main causes of itching in humans are allergies or liver issues.
Chemocare.com does not list itching as a common or uncommon side-effect of Rituxan, meaning that if it occurs, it is in under 9% of all users. If you were to go to the Rituxan official webiste, it is probably 30 pages long, and has a massive amount of information, as required by the FDA.
I ask that you continue to share what you know, since it is very significant for many here -- including me !
max
.
0 -
Yes, it gets to a point where anyone's guessSymptoms
Tgy,
I am convinced that side-effects, in most cases, simply cannot be authoratatively linked to any cause. There may be "best guesses', but seldom certitude. Say a person were to go on just the drug Prednisone, and got agitated and gained fluid weight: that would be a slam dunk -- the Prednisone was the cause. But very few cases are so clear-cut. And most people here are on a collection of chemo drugs and others, and many have the SAME side-effects, and some side-effects occure soon, while others are know to delay for years at times (such as Adriamycine [Rubex] causing heart muscle thickening). So you might never know.
I have been N.E.D. for ten years now from NLPHL, and was never on maintenance. Yet, the last two years, I have had terrible....itching ! Go figure. The N.P. has suggested everything from hot showers to this-or-that as the cause. She is not worried about relapse, and has ordered no scans. I get an annual CBC, metabolic profile, and touch exam, and none indicate any problems.
Many lymphomas take JUST Rituxan for maintenance, and it is a "disease-wide issue, so there is no right or wrong thread to be on. This is fine, or start another -- they are free. I am thankful you have been in C.R. and that the PET shows no real cause for concern. It seems your doctor is following due diligence and watching this with an appropriate level of aggressiveness. He or she, most likely, like us, will never know what caused the itching. But the "other" main causes of itching in humans are allergies or liver issues.
Chemocare.com does not list itching as a common or uncommon side-effect of Rituxan, meaning that if it occurs, it is in under 9% of all users. If you were to go to the Rituxan official webiste, it is probably 30 pages long, and has a massive amount of information, as required by the FDA.
I ask that you continue to share what you know, since it is very significant for many here -- including me !
max
.
Is as good as anyone else's. I.e., I don't think the doctors have any more of a clue than I do on what's going on. I unfortunately am not in complete remission, but have "stable disease." New PET/CT results just came in tonight with SUV uptick of the most active node from 4.6 to 5.6, which compared to some alternatives is fine, but also requires the continuation of the Rituxan, which is increasingly sucking in the side effects it delivers. I'm just wondering why there isn't more literature on late reactions to it...but maybe like the NLPHL I'm just one of those rare cases.
Thanks for your feedback
0 -
R-B in NLPHLNLPHL
Welcome to these Boards, Mary.
About five of us here in the last few years were patients with your strain of HL (Hodgkins's Lymphoma) known as NLPHL. It is the rarest of the five types of HL. Your case must be very early, since the doctors are considering the Rituxan-only approach. I have not heard of that before, but it points out one thing that is unique about NLPHL: It is the ONLY form of HL that Rituxan is useful against. That is, virtually all lymphomas that receive Rituxan are Non-Hodgkin's forms ("NHL"). This is because Rituxan kills a cancer cell known as CD-20, and NLPHL is the only form of HL that stains for CD-20. NLPHL in fact is somewhat of a hybrid form of lymphoma, and for some years in the past oncologists classified NLPHL as NHL, but the worldwide standard today is to consider it an anomoly of HL.
A second curiosity you mentioned is that your oncologist was considering R-CHOP. While I have heard of that a few times in the past, almost everywhere today R-ABVD is first choice agains NLPHL. CHOP is considered a NHL combination, and ABVD an HL combination, but there are exceptions, and this again shows how close NLPHL is to being a NHL form. Finally, your doctors "did not recommend radiation." Radiation is seldom given to advanced stage disease; when lymphoma patients get radiation it is very nearly always either for Stage I or II. Or, the patient with advanced disease will occasionally have a huge mass that needs debulking, and it will be radiated. But otherwise, radiation is little used against any form of HL, so it is not surprising that they recommend not using it, at least at present. I am unfamiliar with Morphea, but it is an example of your doctors wisely trying to do a work-around between diseases.
My own NLPHL was very advanced Stage III, from the collar to the pelvic region, and across both sides.
NLPHL is a very indolent, or non-aggressive lymphoma. Depending on your age and other factors, some doctors think it best to minimize the harshness of chemo for as long as possible. Since Rituxan is usually effective against CD-20, it seems very reasonable to hold back NLPHL with that drug; it may do so for a long, or even a very long, time. My understainding is that Rituxan by itself is not CURATIVE against NLPHL, whereas R-ABVD is regarded as clinically curative, meaning that it will eliminate all traces of the disease for years, usually for forever (relapse following ABVD for NLPHL is 15%, meaning that 85% of NLPHL patients who get ABVD never see the cancer again in their lifetimes).
CHOP and ABVD are both harsh. Rituxan is not a classical chemo, but rather a form of antibody. It too can be unpleasant, but most doctors and patients agree that it is pretty mild compared to CHOP. It will not cause the patient to loose their hair, or most of the other tough side-effects that traditional chemos cause.
I owuld ask the doctors what they think about a few cycles of R-ABVD, toward curative elimination now. They might have compelling reasons to NOT do that. All of us writers here are not medical professionals; we write of what we have experienced, read, and studied. I tell people that "I have no medical training; I have just had all medical problems !"
My summation of all of the above is that Rituxan-only, given the very early stages of your NLPHL, its indolent nature, and your immune system issues, might make Rituxan-only at this time a very sound choice.
I hope you ask more questions and enjoy the fine people here,
max
Mary, I am sorry to hear about your diagnosis. Max and the others have been a tremendous source of support and have openly shared their experiences. My son was diagnopsed last August with Stage 3 NHPHL with B Symptoms. His doctor advised R-CHOP. Because my son is an athlete he was concerned about the potential for cardiac damage so he opted for Retuxan and Bendamustine. The Retuxan is targeted therapy agains the CD-20 protein that is present on the tumor. This protein is the one thing NLPHL seems to have in common with NHL. As Max indicated, Retuxan is not considered curative. The Bendamsutine is more like traditional chemo but does not appear to cause cardiac damage. Though this drug has been used extensively in Europe it is not usually recommended here in the US. We discussed it with the oncologist and he felt that it was a "reasonble" choice. The large messenteric tumor shrunk immediately following the first round of chemo to the point that it was not palpable. The other smaller tumor under his arm also shrunk and his symptoms improved. We have two more rounds to go and am hopeful he will have a complete response and NED in the near future. Max is a great source for sharing his experience and has helped us tremendously.
0 -
R-BendekaGalllessgal said:Just diagnosed with NLPHL
Hello!
First off, I can't tell you how amazing it has been to find a board focused not only on those diagnosed with NLPHL, but those who have had lymph node enlargement in their mesentery. From much of the reading I've done and from what my oncologist has told me, it's really not as common for this disease to present in the mesentery, so it has been reassuring to know that I'm not the only one with this uncommon presentation.
A little background: I've been dealing with illness and inconclusive symptoms for a few years now, the main two being extreme bouts of fatigue, and bouts of diarrhea that have become more frequent over the past three years. I also have had a slew of colds and seemed to be able to get sick quite easily, or at least easier than in the past. I only really started to feel incredibly sick in January of this year, with severe abdominal pain, nausea, lightheadedness, more fatigue, and more intense bouts of diarrhea paired with bouts of constipation. I do have a history of GI issues including gallstones and resulting pancreatitis (gallbladder removed in 2012), stomach ulcers, and GERD, so my GP and GI put me on a massive dose of PPI's and told me to hold out for a few weeks while they started to work.
Lo and behold I didn't feel any better after a few months, so I went back to my GP in tears saying that I just don't feel right and I really feel like something more must be going on. She ordered a CT and in April I was diagnosed with a mesenteric mass; a PET CT one week later showed inflammation or disease in the 3.3cm mass and was told that it looked like I had a carcinoid tumor (especially based upon my symptoms). The PET also showed up to a dozen other enlarged masses, but they were not exhibiting disease or inflammation in the scan.
After consulting with a specialist in neuroendochrine tumors and having a specialized gallium dotatate PET scan in early May, I came back negative for that type of tumor and was back to square one. Mind you that at this point, none of the oncologists or other specialists that I had consulted with had thought this could be Lymphoma. I'd already felt nuts because these symptoms are so common from many other, less scary disorders; after being told I didn't have a carcinoid tumor I started to wonder if this was all in my head.
My surgeon convinced me that the only way to really know what this mass was is through surgical removal, so on 5/17 I had laprascopic surgery to remove the mass - a week later on 5/22 my surgeon called saying that it looked like I had a rare version of lymphoma. Two days later I saw a hemotologist oncologist aat UCLA who finally diagnosed me with NLPHL. While the blow of a cancer diagnosis was huge, for the first time in months (or years, really), I finally felt like I wasn't crazy, that the fatigue wasn't just me being lazy or not taking care of myself. It's been freeing in a way.
I will be starting a BR regimen (Bendamustine and Retuximab) in the next week or two - four three week cycles followed by a PET scan to look for disease, then up to two more cycles if needed. Bendamustine doesn't have a clear record of causing or not causing damage to the ovaries, but to be safe we are highly considering egg retrieval prior to starting chemo since it does contain alkylating agents. My oncologist, who I trust implicitly, said that in recent studies BR has an over 90% success rate (100% in some studies) at treating NLPHL, and is much better tolerated than R-Chop or R-AVBD by most patients, with far fewer side effects. What really hit home was when he told me that I'd likely feel better after the first dose of this protocol than I have been feeling over the past few years.
I'm wondering, did no one else's doctors discuss BR protocol with them as opposed to R-CHOP and R-AVBD? It was such a straighforward decision for my doctor, but the factors of age (I'm 33), the fact that I want to have children, and disease stage may have been an influence in his decision.
As far as radiation, it was a moot point in the discussion of my care since my largest mass was in my mesentery and it has now been removed. It also sounds like targeted radiation is pretty impossible for mesenteric masses because of their location. Has anyone heard differently?
Has anyone else had any overt symptoms related to their NLPHL? Sounds like many people just find a mass and go from there. Anyone else with fatigue?
Hoping everyone is doing well with treatment and I so appreciate any insight compared to your own journeys!
Sonja
My 45 year old son was diagnosed with NLPHL in August after a year of symptoms and misdiagnosis of acid reflux. He had Stage 3 NLPHL with B Symptoms. Large mesenteric 4 cm tumor. Needle biopsy. Took 4 patholgists to review before calling a diagnosis. He came here to ask about experience with various regimens. His doctor recommended R-CHOP. After much consideration he went with R-Bendamustine due to the overwhelming clinical experience in Europe and the fact that it does not cause cardiac damage. It is still no walk in the park, but his messenteric tumor responded almost immediately after the first round of therapy and his symptoms lessened. He starts two consecutive days of round 5 tomorrow. Treatment is long for the first round but now he is on rapid infusion and is in and out of the infusion center in 30". I hope this helps. Good luck with your treatment.
0 -
NLPHLIluvlucy said:Website crash booted me out.
I got booted out with the website crash. I'm early on in my NLPHL journey. I have met some of you in this discussion board and it has been very helpful to network with others. I was dx with NLPHL on 1/2/2019. Had CT of chest/abd/pelvis and PET. Have been staged at IIIA due to positive nodes in my right armpit and mesenteric nodes. I've never felt sick, in fact feel fabulous physically. I haven't missed a day of work in over a decade, no colds, flu, etc. I found a lump in my R armpit this summer, which is the same area that had a core needle biopsy 4 years ago and came back "normal". Fast forward 4 years later I have this lump. Doc wanted to do a mammogram first that came back normal. I was supposed to have an ultrasound done at the same time but the imaging dept refused to schedule it until the mammo results were in and then they were to call me to schedule, but they never did. Meantime, my husband and I found our dream home and within 24 hours had an accepted offer and the process of mortgage and move occupied my mind and time. Once we were settled in I reached out to my doc and got the ball rolling again. Ultrasound showed large nodes, so had them excised and the path report came back positive for NLPHL. I have not agreed to any treatment at this time as I am in the process of getting 2 more opinions at large cancer centers. I am a nurse in the industry and am having to do far more advocacy for myself than I thought I would need to. I have to double check everything that professionals and staff say they are going to do as I have found too many miscommunication and assumptions that have delayed my workup and interrupted my path to treatment. I just had to call the cancer center that my Hem/Onc wanted me to have a second opinion at and the treatment center hadn't contacted me in days. When I talked with the nurse assigned to my case, she told me that she didn't move forward with my referral as she thought I had already started treatment and she also thought I was dx with classic hodgkins lymphoma. I'm frustrated at this point. I don't want to go down the path of traditional chemo as I know these drugs, I've administered these drugs and am terrified. I don't want to lose my hair and am tired of people saying "it's only temporary". That minimizes my feelings and makes me angry. Hair loss is demeaning to me, and I won't be able to work full time, so in essence I will feel sick, have my paycheck affected and lose my dignity for this cancer that if not for the lump, I'd have never known anything was abnormal. Anyhow, that's my story and my rant. I'll get through this but am not looking forward to the next 6-8 months of my life. I have a very strong faith and an incredible posse of family and tons of friends who have worked in hospitals with me, oncology, hospice, and Palliative Care for the past 31 years. If you've made it through my post to this point, bless you, you have patience.
Paula
Paula, We had a similar experience with the right hand not knowing what the left hand was doing. I am in the industry of CV medical sales and am a Medical Technologist. I was surprised at the amount of self advocacy we had to do to get a correct dx for my son. Ultimately after a year of insurance denials and appeals we were able to get approval for an MRI which confirmed the suspicion of lymphoma an the needle biopsy was almost a joke. QNS so it took multiple paths to call the dx. Ultimately my son went with the less toxic R-Benda and is almost done with tx. Side effects are progressively worse with each round, but no hair loss and no CV AE's. Tumor response was good almost immediately and symptoms subsided. I hope that helps. Good luck.
0 -
SuperPaula Camille said:NLPHL
Paula, We had a similar experience with the right hand not knowing what the left hand was doing. I am in the industry of CV medical sales and am a Medical Technologist. I was surprised at the amount of self advocacy we had to do to get a correct dx for my son. Ultimately after a year of insurance denials and appeals we were able to get approval for an MRI which confirmed the suspicion of lymphoma an the needle biopsy was almost a joke. QNS so it took multiple paths to call the dx. Ultimately my son went with the less toxic R-Benda and is almost done with tx. Side effects are progressively worse with each round, but no hair loss and no CV AE's. Tumor response was good almost immediately and symptoms subsided. I hope that helps. Good luck.
Delighted to see your report regarding Chris. Please do not be a stranger
0
Discussion Boards
- All Discussion Boards
- 6 CSN Information
- 6 Welcome to CSN
- 122.1K Cancer specific
- 2.8K Anal Cancer
- 448 Bladder Cancer
- 309 Bone Cancers
- 1.6K Brain Cancer
- 28.5K Breast Cancer
- 398 Childhood Cancers
- 27.9K Colorectal Cancer
- 4.6K Esophageal Cancer
- 1.2K Gynecological Cancers (other than ovarian and uterine)
- 13K Head and Neck Cancer
- 6.4K Kidney Cancer
- 673 Leukemia
- 795 Liver Cancer
- 4.1K Lung Cancer
- 5.1K Lymphoma (Hodgkin and Non-Hodgkin)
- 239 Multiple Myeloma
- 7.2K Ovarian Cancer
- 65 Pancreatic Cancer
- 490 Peritoneal Cancer
- 5.5K Prostate Cancer
- 1.2K Rare and Other Cancers
- 543 Sarcoma
- 738 Skin Cancer
- 658 Stomach Cancer
- 192 Testicular Cancer
- 1.5K Thyroid Cancer
- 5.9K Uterine/Endometrial Cancer
- 6.3K Lifestyle Discussion Boards