ABVD didn't work

So I've had a bit a horrible year to say the least. Graduated college with and bachelors of science in May 2016 (at 47- finally!) got a seasonal job doing a federal geological/ soil infiltration study that paid well, thinking my life was finally on the upswing. Then my fiancee of 10 years breaks up with me (she lost her mind and former sweet personality to oxycodone addiction from a surgery) I had to move out of the house (her parents bought her) and move in with my family in PA (from Buffalo). Reeling, I began the long process of living out of boxes, trying to find work, when a series of ailments struck me.
At first I thought I picked up a weird peronchia (nailbed infection) from the gym I was attending in November 2016, but then a month later developed cellulitis on my lip that did not clear up for weeks. I tried to explain to the Patient First doctors (my PA insurance did not kick in till March) that a year prior in March of 2016 I developed and abscess under my left armpit and it was drained but when I went back to have an ultrasound to see where the residual sac was to be removed they could not find anything. I kept asking if maybe I suffer from an auto immune disease because 3 infections requiring powerful antibiotics to beat them in one year? I mean I'm not a doctor but do have a scientific background and I knew there had to be a connection. Everyone, including people in my family thought I was just stressed from my traumatic year.
In late May/ early June of 2017 (can't remember really) on a hot day I was wearing a tanktop and noticed my left armpit (same place I had a abscess over a year ago) was really swollen. I made an appointment with my PCP and he took a look at it and referred me to a Einstein Network for an ultrasound and male mammogram. I had 3 male mammograms that day (I have a whole new level of respect for what women have to endure with those!). The doctors there said they were going to refer me to a surgeon at Einstein. She turned out to completely change my mind on the medical profession. See my whole life I've never really been sick, exercised, never smoked, ate relatively well, and going through all these tests were really starting to make me feel like it was a complete insurance money grab. I was like surely this is another abscess just drain it already and figure out what auto-immune disease I have? Turns out this surgeon saved my life I think.
When I went to visit her Dr Schermer thought I might be right about the abscess. She saw the scar where one was drained the year before but told me the ultrasound didn't show much and ordered a CT Scan. Later on I found out, right then in there (when she saw the CT Scan) she knew it was Hodgkins but did a fine needle biopsy to be sure. Unfortunately (and again she called it) she knew it would be non-diagnostic because the lymph nodes were so swollen she only got fatty tissue and no lymph node tissue. So in one sense I was relieved that it proved non-cancerous but she was determined to get a real diagnosis. She scheduled me for surgery to remove a lymph node for testing (something she was completely against at first because she said lymph node removal is the last resort). I have never been under in my life so I was terrified.
I told her in recovery not to sugar coat anything and she can call and give it to me raw over the phone either way. I got a call a few days later- Hodgkins Lymphoma but assured me she thinks its in an early localized stage and highly treatable! I went through all the normal emotions people do when I was in shocked, I cried, wondered how this could have happened? Dr Schermer then recommended me to a oncologist/hematologist at Einstein.
The night before my oncology appointment my family had left for the shore and I was home watching a movie with my mother who has early onset Alzheimers. I began feeling chills and feverish at the same time and kept thinking is this a symptom of Hodgkins? I went upstairs to get a sweatshirt (it was really hot out so I was a bit freaked out) and noticed my underarm incision was bleeding and even more swollen. 9 days post surgery and it was severly infected (and till this day- 42 days later has not fully healed). My mother was frantic and my aunt and uncle came over in the morning (I had called my surgeon already but did not get a response) to take me to the oncology appointment. I got there with a 104 temperature- they called my surgeon and said she needed to see me right after my appointment to address the wound. My oncologist Dr Tester told me I have NLPHL (Nodular Lymphocyte Predominant Hodgkins Lymphoma) and he believed it was early- stage 2A, since I had no B symptoms. By then I also had developed swollen lymph nodes in my left neck area. He scheduled me for a Pet Scan and 2D Echo Doppler (test my heart health) for staging/diagnosis 8/31/17.
Turns out they had to get pushed back. My infection was so bad I had to go to my surgeons office every day for weeks so she could pack it (keeping the wound open and draining) and change the dressing. Underarm dressings are the worst. I was so freaked out I had this open wound under my arm. It was hard to sleep, then I developed an allergic reaction to the tape used and bleeding blisters formed all around the wound. I was taking 2500mg's of 2 antibiotics daily for a month. It seemed **** Hodgkins was the least of my problems!
Finally after Labor Day I stopped getting dressing changes and said **** it: This has to close because I can't deal with it. My Pet Scan/ 2D Echo were rescheduled for 9/14. This entire time I had been googling about my Hodgkins, reading peer reviewed literature, but unfortunately my results came through on my patient portal before the doctor made an appointment follow up. All I saw was 'Advanced Hodgkins' on the report and I knew it would be bad. I knew it would be bad because also since the infection started clearing up I developed a bunch of 'B' symptoms: Drenching night sweats every night, fevers/chills not associated with the infection, I lost 10 pounds and my appetite, worse thing is now I have this dry persistant cough I presume because nodes are pressing on my lungs. I wrote down a ton of questions to ask including will I be given R-ABVD for treatment? I met with Dr Tester on 9/22 for staging/ treatment plan. He was surprised but gave it to me straight, initially though to be stage 2A but now is stage 4B. I looked at the Pet Scan and it showed not only the large masses of infected lymph nodes in my left armpit/neck region but the Dr pointed out how there were osseous lesions all down my spinal column and my right hipbone and my spleen is slightly enlarged FDG Avid, and indication of infected lymph node above and below the diaphragm. He said he was shocked but it looks systemic.
Now I'm a tough person. I've been through a ton of **** my whole life including being homeless for 6 months when I was 24. I can get used to any bit of bad news including cancer but this whole thing from the onset would never let me just get comfortable. No sooner than I started using my dry sense of humor on my condition to psyche myself up for upcoming treatment did it just get a whole lot more serious!
I can't lie, I'm scared as **** now. I go back an forth btw I'm going to kick this things **** to- **** what if I can't?. I start 6-8 months of R-ABVD on 10/6. Only bit of good news is Dr Tester says physically I'm really fit for my age, my heart is healthy, and I have a positive mental attitude about it- which he says goes a long way into beating this and being cured. He says really the only thing bad you have is stage 4B and you're male on the unfavorable list. I get a port this week I think (thankfully it's not put me under surgery again!) but I'm worried about treatment. I mean I know I need it (and thankful Rituxan is included as a monoclonal antibody!) but man the cure sounds worse than the disease! I keep thinking I'm going to come out of this feeble, with a bad heart and lungs, and will it work? I already feel fatigued from the advanced Hodgkins (NLPHL)
Anyhow I went to the chemo ward on 9/22 as well and met some of the nurses. I said hi to a patient and said "I'm about ready to join your club!" He said it's only a fun club to join if you get to leave eventually.
Comments
-
Unique
Welcome to you here Lixx. You will be needing that gung ho attitude for the next year.
We went many years here with almost no NLPHL patients (except for me and a few others), but in the last year, have had a deluge of them. If you look back through the treads begun in the last year you will find them, and all are worth reading for you. And no, NLPHL is not becoming more common than before -- there is no evidence of that. It has been around as long as Lymphoma itself.
If you look back through my posts over the years, you will see that what I am about to share with you below I have shared before 100 times with others. But neither they, nor I, much feel like digging back through all of that. The regulars and old-timers will either ignore those memories, bear with us here, or simple skip my "NLPHL Intro."
Much in your diagnosis reminds me of me. A bit older at diagnosis than is normal for NLPHL (you 47, I was 53). Advanced disease, NLPHL is ordinarily discovered at Stage I or II. I was a heavily involved Stage III-B, you a IV-B. So yes, you have at least 2 "Unfavorables" in your chart. Other Unfavorables could be specific blood test values, and a few other variables. This lowers predicitions for so-called Five Year Freedom From Disease (FFD) estimates, but do not dispair, since even with Unfavorables, NLPHL remains very beatable. Your percentile liklihood of being FFD in five years is still over 50%, since my estimate at diagnosis was ~60-65%. This might not seem like a new Cadillac on Christmas morning, but believe me, there are many worse scenarios written about here weekly. I remain FFD at approximately 8 years now.
Another recent spate is that many of the people presenting with NLPHL have atypical or subvariant disease. That is their NLPHL is not "normal" NLPHL, but has T-Cell or other odd-ball involvement. This means that you need the absolute best and most conclusive pathology/diagnosis possible. I recommend that your biopsy be reviewed by at least one additional pathology lab. Even though you sound a bit strapped for cash, I recommend you get the insurance to agree to this. Your prolonged issue with recent infections suggests to me that you may have other autoimmune issues, which should be ruled out.
R-ABVD is indeed the current gold standard for NLPHL. It is first choice among probably 90% of the Hematologists in the US (an approximation on my part), as well as England and much of western Europe. Since you are as you state in very good shape going in, you will come out a bit worse for wear, but should maintain normal heart and lung function.
The two worst drugs in ABVD are Adriamycin, which in about 2% of users causes delayed thickening of the heart muscle, which mimics congestive heart failure (CHD). Symptoms of this can be delayed as long as 7-10 years after use. But 2% is a pretty small number, and Adriamycin is also in most of the other alternative durg combinations; it is in R-CHOP and R-EPOCH, for instance.
Bleomycin is the other worst bad boy in ABVD. It causes lung toxicity of various forms in around 10% of all users, but ordinarily, this toxicity passes after treatment ends. But, it causes lung fibrosis in 1 to 2% of all users, and fibrosis is permanent. I have fibrosis, but the cause was never absolutly linked to Bleo, but my toxicity surely was. Signs that serious toxicity are beginning are severe cough that will not stop (at least it does manifest warning signs at the beginning). Bleo is NOT in CHOP. Bleomycin toxicity chances increase with age, previous application, and previous lung disease. But it can occur in any user.
The third most common problem on ABVD is that the Vinblastine will routinely cause neuropathy, or numbness in the hands and feet. Usually this is mild, at other times severe. Usuually it passes after treatment ends, sometimes it does not. Mine came down in the severe and permanent categories. Vinblastine or its sister drug Vincristine are also in CHOP, EPOCH, and most Lymphoma cocktails.
Rituxan is only effective agains NLPHL among Hodgkins-type Lymphoma. No other HL receives Rituxan, making it ordinarily a NHL drug only. But it is of great vaule against NLPHL.
NLPHL is nearly always put into full remission by first-line treatment. But again, we have recently had two cases that were not. Overall, NLPHL, once in full remission, never reoccurs for around 85% of patients who entered full remission. That leaves the other 15%. Chances of remaining in full remission are better for people who finish all of the scheduled treatments, since residual cancer cells undetetable on PET or CT must be killed off completely. I did 6 cycles, or 12 infusions, of R-ABVD, which is 6 months of tretment. I was in or near full remission by the 4 month mark. But ending my treatment then would have been a very ill-advised move, for me or anyone else with indolent Lymphoma.
You should emerge from this a winner. Most people do. Expect by the end of the second infusion extreme fatigue and weakness. I needed assistance with my daily affairs by that point, but not all do,
max
0 -
thanks max
Thank you so much for all that info Max! I read a bunch of those threads before signing up and I knew I was in the right place. I'm not 47 anymore though lol. I turn 49 on October 1st this year. Sorry I started my horror story in late May 2016 when I was turning 48 in 4 months. So yeah cancer is NOT the gift I wanted when I turned 49! But silver lining? If I turn 50 cancer free I'll be a happy camper.
My blood tests came back really well- albumin etc. So that's also a bit of good news if any can be found.
Since I was unable to find work I had to go on Medicaid in March 2017 and to be honest even though I'd rather have a career and be working I've never been more thankful for it. I can't imagine what these bills would be like without the assistance. I mean the ultrasound, mammograms, ct scan, pet scan, 2d echo, surgery, bisopsies.....I'd be hurting big time. Sucks I have no income but my whole life I've never used assistance and having it came just at the right time.
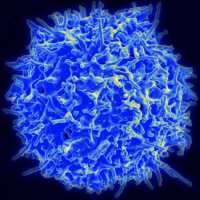
I honestly think those infections were the start of my Hodgkins to be honest. I only developed swollen lymph nodes around May of this year. There is no way since May it could have advanced to stage 4B since this particular Hodgkins moves at a glacial pace. Unless I have some hybrid aggressive form. Doctor Tester said I had no Reed Sternberg cells and CD20 was what he found. I mean maybe all those infections were my immune system trying to fight off the cancer then I finally got swollen lymph nodes which alerted me something was really wrong?
I'm already pretty fatigued like I have the flu (but then again I just got a flu shot over the weekend as a caution before starting chemo) but I think I'm going to order more Death Wish coffee to help with that!
0 -
Lixx you young man and I read all of Max's post.
Well you heard from Max and I have little to add. I also had or have NLPHL . I say had because I am waiting to find out if indeed it has come back. I was diagnosed at 52 and started treatments on my birthday in March of this year. I was 3B and lost 42 pounds. I was one that had RCHOP because it had transformed into NH T Cell rich B cell aggressive Lymphoma. I did not think the first 4 treatments wereweeks too bad. The last 2 I was worn out. Then 6 weeks after the final treatment life started getting back to normal. I still have a way to go but at least the severe fatigue that started before treatment is gone.
I should find out in the next month if it is back and what to do.
Wishing you the best. There is a lot of support on this forum so come and ask questions and share anytime.
Sandy Ray
0 -
Hey Sandy Ray!
Well here's to hoping your NLPHL is gone for good sir! Wow 42 pounds? Was it because you just had no appetite at all from the Hodgkins or treatment? My Hodgkins seems to have made me never hungry, but I force myself to eat- and I'm trying to eat a bit healthier. I mean I joked (I have a bit of self deprecating sense of humor) to my closest friends that I'll probably drop that 20 pounds thanks to Hodgkins I could never seem to lose but wow I'd be nervous losing that much. I went from 202 to 192 in the last month.
That's very promising that you said the severe fatigue that started before treatment is gone. It's very depressing. I was a pretty active person but sometimes I just lay in bed because I'm just so damn tired! I hate it.
0 -
If pathology is nailed down
Sorry to welcome you here! But, as you can see, correct pathology is crucial to proper diagnostics, and diagnostics are crucial to proper treatment. Proper treatment is necessary for the best outcome. But, it all follows from correct pathology. NLPHL is one of the odd ducks of lymphoma - which is an odd duck in the cancer world. CD20 nails it down as a B-Cell Lymphoma, since CD20 defines a B Cell. That much is good, since some extremely rare occurrences of Hodgkin's are of T-Cell origin rather than B-Cell, which can greatly complicate things. You can also see that, lacking Reed-Sternberg cells, its identity as a Hodgkin's variant is in questiion. It seems to be related to a precursor of Diffuse Large B-Cell Lymphoma in certain cases. As with many lymphomas, the picture simply is not all that clear.
As to prognosis such as Karnofski score, International Prgnostic Index and the other predictors, they attempt to be predictive and statistical in nature, meaning that they apply to exactly no one. They meausure possible outcomes only. In truth, we each form our own survival curve and prognosis. I guesstimate that I have about a 1% chance of being alive after nine years of what began as a poor prognosis and dropped immediately, and several times since. I choose not to pay attention to the prognostic indicators.
Some tend to panic once they are placed on a salvage regimen, thinking that it is near the end. Well, it was my 5th salvage regimen, seven years into this battle, which placed me in full response. And that was after two relapses, a mutation into two subtypes, and a secondary marrow cancer (MDS) caused by extensive treatment. We hear a lot these days about "Outliers" - those who are outside of the norm; exceptional cases for various reasons. Aim to be an outlier, as you will not achieve that status unless you aim for it.
0 -
LixxLixx said:Hey Sandy Ray!
Well here's to hoping your NLPHL is gone for good sir! Wow 42 pounds? Was it because you just had no appetite at all from the Hodgkins or treatment? My Hodgkins seems to have made me never hungry, but I force myself to eat- and I'm trying to eat a bit healthier. I mean I joked (I have a bit of self deprecating sense of humor) to my closest friends that I'll probably drop that 20 pounds thanks to Hodgkins I could never seem to lose but wow I'd be nervous losing that much. I went from 202 to 192 in the last month.
That's very promising that you said the severe fatigue that started before treatment is gone. It's very depressing. I was a pretty active person but sometimes I just lay in bed because I'm just so damn tired! I hate it.
Well the weight loss was from just a loss of appetite. I am a small person who was a little overweight. I weighed about 198 starting out. My dream weight was 165 which was no problem. Great weight loss regime. I am now back up to about 170. I could not imagine ever being hungry again. I am now starving almost 24 /7. Unfortunately my metabolism has not increased. So I have to curb my eating some. Loss of appetite was from Lymphoma mainly. Near the end of treatment was from the Chemo. If you can keep your muscles active. My atrophied terrible and I have a lot of work to do to get that back. Not like I was muscular before but now I have very little strength . I feel good but I cannot lift or climb very well. If I do try and do anything it will wear me out. Oncologist said that would take about 6 months. He has been dead on for the most part. I was more patient with treatment than recovery. Although just feeling good and feeling like getting out and about is the most important.
Keep us posted.
Sandy Ray
0 -
More set backs
I went to get my port put in today but they could not do it. I developed an abscess under my left armpit towards my left nipple and have been taking Keflex (luckily I had a bottle of 56 capsules from August) for 4 days straight and did not have to deal with a emergency room visit over the weekend. And while it appears to be healing up the surgeon would not do it (rightly so) with an infection so close to where it would be. Can't delay treatment anymore so he talked to my Onc and they settled on a double pic line for now.
My chemo schedule is super weird. They are just doing Rituxan tomorrow and ABVD on Thursday. Reason being they said in advanced cases with first time Rituxan usually there is a strong reaction and its a long drip. The weird part is they have me scheduled for the 13th and the 20th. I thought I was supposed to get a week off in btw chemo cycles?! Maybe since I've had so many delays and the 4B diagnosis they really want to get going?
0 -
ChallangesLixx said:More set backs
I went to get my port put in today but they could not do it. I developed an abscess under my left armpit towards my left nipple and have been taking Keflex (luckily I had a bottle of 56 capsules from August) for 4 days straight and did not have to deal with a emergency room visit over the weekend. And while it appears to be healing up the surgeon would not do it (rightly so) with an infection so close to where it would be. Can't delay treatment anymore so he talked to my Onc and they settled on a double pic line for now.
My chemo schedule is super weird. They are just doing Rituxan tomorrow and ABVD on Thursday. Reason being they said in advanced cases with first time Rituxan usually there is a strong reaction and its a long drip. The weird part is they have me scheduled for the 13th and the 20th. I thought I was supposed to get a week off in btw chemo cycles?! Maybe since I've had so many delays and the 4B diagnosis they really want to get going?
Sorry about the port delay Lixx. A port can be installed either side of the chest (L or R), but I understand the surgeon's hesitancy. A PIC Line sucks -- very inconveneient. I would push for the port install at the first opportunity.
R-ABVD is usually given all at once (same sitting). But oncologists vary this stuff as necessary. Usually, R-ABVD is once ever 14 days. But do not let it bother you, they know what they are doing.
Rituxan is a LONG BAG. My Rituxan bag was a good 3 hours, even later on, after I got used to it. My infusion day was 8 hours: I got there about 7:45 AM, and left at about 4:00 PM. This can be a marathon, and by mid-day I was dragging my IV tree to the restroom every 20 minutes; it is a huge amount of fluid. It might be advisable for a patient to break this up a little if there is clinical reason to do so. Other combos require inpatient delivery, so do not fret. My 8 hour day was despite the fact that, according to my infusion RN, I got all of the drugs "wide open," or max rate.
I do not think 4B is a factor, since R-ABVD will do about the same thing for a 4B patient that it will do for a 2B.
Another part of your routine will be going for your Neulasta shot, the WBC stimulant. This has to be at least 24 hours after the AVBD portion, but withn 48 hours, so the 'window' is small. I do not think that the Rituxan would factor in to what day the Neulasta is given; it is a tiny needle shot usually administered on top of the belly. Painless.
Continue writing and asking all questions that occur to you big guy,
max
0 -
Coping with your PICC
Hi Lixx...Sorry things are not going as smoothly as you would like, but hopefully everything will be sorted quickly. A couple of suggestions for dealing with your double-PICC (I had mine in for 5+ months). 1) get some "tubular net dressing" and cut a segment to hold your PICC ports from flopping around. This will keep you more comfortable at home. Be sure to relocate them under the dressing frequently so as not to get sore spots underneath the caps. 2) Coban stretchy material is also useful while getting chemo. Wrapped around the ports in just the right place can keep the nurses from inadvertently tugging on them. Good luck with everything.
Another helpful thing if you are going to be in-hospital: I took a bathrobe, sliced open the shoulder and arm to put in snaps on the PICC line side. That way, I did not have to disrobe every time someone needed access to my PICC...Which was frequent! You can buy clothing that does this, but it's expensive. I found a $10 robe and just fixed it up.
0 -
@Max- you weren't kidding!
@Max- you weren't kidding! Started at 8:30am ended at 4:20PM. They gave me Benadryl and Tylenol to counter the adverse reactions since it was my first time. Slow drip at first 20- then 40 then I got to 128. Smooth sailing they couldn't believe I wasn't having any reactions. But that all came to a standstill. At 1:30 I developed a chill I could not get rid of (rigors? I believe they called it). I was shaking uncontrollably even with 3 heated blankets on me. A team of nurses and my Onc quickly came over- I had a temp of 103.7 (and super cold). Pumped me with a steroid, more tylenol, and benadryl. Soon I was a furnace and peeling layers off. Good news is that means the Rituxan was doing it's job on the CD20! I feel better as I'm writing this and not coughing as much at all. My oncologist believes after 6 treatments I might be in full remission and my symptoms will be alleviated (night sweats, chills, fevers, cough).
Oh he said he's doing the Rituxan every week for 6 weeks that's why it seems like I have chemo scheduled each week. The ABVD part which I begin tomorrow at noon is every other week.
@Evarista- yes I did get that tubular net dressing-it's a lifesaver! I don't mind the pic line for now because I needed to start my treatment which had been delayed already by a month but I'm really looking forward to getting it taken out and the port put in! Hopefully this abscess infection disappears in a week or so. I already was told I'm going to have to have a home helath aide come over and flush the pic line starting Friday. Good news is they'll show me how so that will be short lived hopefully. I mean I saw it today and I did it for someone 20 years ago so I should be able to.
0 -
Rituxan
My Rituxan was given the first treatment by itself and the next day I had my Chemo. First day of Rituxan was 8:15-5:00 a long day for sure. It did great though. The tumor on the outside melted away and I assume the ones inside were doing the same. I did not have any reactions after the first treatment. Wishing you the best. Eat whenever you can and lots of fluids. Fluids are most important especially on the first treatment to prevent tumor lysis.
I was like Max after they pushed all that fluid I got lots of exercise pushing that IV pole back and forth to the restroom.
Glad to hear your updates .
Sandy Ray
0 -
Common with RituxLixx said:@Max- you weren't kidding!
@Max- you weren't kidding! Started at 8:30am ended at 4:20PM. They gave me Benadryl and Tylenol to counter the adverse reactions since it was my first time. Slow drip at first 20- then 40 then I got to 128. Smooth sailing they couldn't believe I wasn't having any reactions. But that all came to a standstill. At 1:30 I developed a chill I could not get rid of (rigors? I believe they called it). I was shaking uncontrollably even with 3 heated blankets on me. A team of nurses and my Onc quickly came over- I had a temp of 103.7 (and super cold). Pumped me with a steroid, more tylenol, and benadryl. Soon I was a furnace and peeling layers off. Good news is that means the Rituxan was doing it's job on the CD20! I feel better as I'm writing this and not coughing as much at all. My oncologist believes after 6 treatments I might be in full remission and my symptoms will be alleviated (night sweats, chills, fevers, cough).
Oh he said he's doing the Rituxan every week for 6 weeks that's why it seems like I have chemo scheduled each week. The ABVD part which I begin tomorrow at noon is every other week.
@Evarista- yes I did get that tubular net dressing-it's a lifesaver! I don't mind the pic line for now because I needed to start my treatment which had been delayed already by a month but I'm really looking forward to getting it taken out and the port put in! Hopefully this abscess infection disappears in a week or so. I already was told I'm going to have to have a home helath aide come over and flush the pic line starting Friday. Good news is they'll show me how so that will be short lived hopefully. I mean I saw it today and I did it for someone 20 years ago so I should be able to.
Lixx,
I have talked to a lot of nurses about Rituxan over the years. In fact with my long-term followship RN last August. She said that years ago she was on the team that gave the first-ever Rituxan infusion at my cancer center, which is linked to a teaching hospital, today about 30 oncologists. I don't remember the year, but Rituxan is not a new drug, around a "long time," at least in "oncology time."
She said that about 5 minutes in, the patient went into full arrest, but was brought back readily. That patient later was able to get Rituxan as necessary. Severl writers here have experienced full arrest from Ritux.
These frightening episodes are almost always linked to the first infusion. Much less likely thereafter.
As I wrote above, I started slow on my first infusion, but was going "full blast" before the end of that bag. And full blast thereafter.
However I got severe chills EVERY INFUSION -- all 12. This usually began almost as soon as the infusions began, and were over within less than 30 minutes.
max
0 -
Got through the first chemo
Got through the first chemo on Thursday. Much shorter day. Developed a fever of 102 when I got home was freaked out lying in bed having trouble cooling down- my family called the hotline for Einstein and they told them to give me tylenol (which me and my brother in law argue about all the time since I'm an avid Advil user- it just works on me best). Finally got to bed (heatwave here wasn't helping as we packed all the AC's away).
Next day I felt tired but much better and no fever. Today I'm a bit queezy so I popped an anti nausea med they gave me just in case. I have two diiferent home health aides coming one came yesterday to show us how to flush the pic line and will be back Tuesday to change the dressing around it, and I assume the other coming Monday is going to check on the abscess that is almost healed I guess? I really can't wait to get that port so all this extra work at home can stop.
Good news is my cough has stopped, night sweats aren't as crazy, and I feel like all those lymph nodes in my neck, chest, and left armpit shrank a little at least. Bad news- I'm scared my immune system is shot and I'm drained but trying not to think about the downsides of chemo too much. I have eaten loads of protein and some fruit. Plenty of water as I've been peeing like a racehorse. Which is good to flush those chemo drugs out along with dead cells I thnk.
0 -
Rituxan
My first time getting it seemed to be going very smooth. I don't remember how long it was until the roof of my mouth felt weird. When thenurse came in the feeling went away. She took vitals and as she did so that weird feeling came back. Right away another nurse came in and they agreed to treat it as an allergic reaction. Since then the worse I get is restless leg but that is likely from the high dose of th benadry and goes away as soon as the Rituxan is started.
I not only had Rituxan as part of my 6 cycles of R-Chop but also with 3 cycles of RICE and now the 2 year maintenance period. It is so routine it is now my Spa Day, day off from work.
0 -
Update
So I've had 5 Rituxan treatments and 2 ABVD treatments (1 cycle) so far. This Friday is my last Rituxan and then ABVD so it's a long long day in the chair. I had some serious issues after first chemo and had a string of staph infections (boils) which again delayed my port placement. Then my ABVD got cancelled one week because my either my ANC or WBC was too low (.4 I was told!) Oncologists started me on the Neulasta shot and this has stabilized my counts to almost normal. I finally had the pic line removed and got the port.
The Oncologist is happy with my progress after a rough start. Obviously no re-scans have been taken but he feels the lymph nodes are really retreating which is a good sign. I'm skeptical because this week some in my neck appeared to swell up and shrink again and it's happened a few times. Night sweats are also coming and going, where before they seemed to be starting to subside (never completely). Is this normal for the nodes and sweats to almost go away then come back and start to shrink and go away again?
I honestly won't be super optimistic till I see a new petscan which I guess won't happen till I've had a few cycles of ABVD. The doctors think that if I'm really improved they might dial back some of the harsher aspects of ABVD drugs to lower doses. My main concern after initial diagnosis (4B) was the Hodgkins in my vertebrae, spleen, etc. I can feel the nodes getting smaller (despite that one in my neck) and my Hodgkins symptoms (cough, no appetite, fatigue etc) have subsided, but I can't look inside myself to see if the spleen, vertebrae have gotten better.
Side effects from treatment have been pretty minor after the initial shock to the system. My beard thinned a lot. Body hair doesn't grow (I'm kind of happy about these lol- low maintence), fatigue is still major after chemo for about 4 days. I had horrible heartburn but never nausea. I'm taking prilosec for that now.
0 -
OverallLixx said:Update
So I've had 5 Rituxan treatments and 2 ABVD treatments (1 cycle) so far. This Friday is my last Rituxan and then ABVD so it's a long long day in the chair. I had some serious issues after first chemo and had a string of staph infections (boils) which again delayed my port placement. Then my ABVD got cancelled one week because my either my ANC or WBC was too low (.4 I was told!) Oncologists started me on the Neulasta shot and this has stabilized my counts to almost normal. I finally had the pic line removed and got the port.
The Oncologist is happy with my progress after a rough start. Obviously no re-scans have been taken but he feels the lymph nodes are really retreating which is a good sign. I'm skeptical because this week some in my neck appeared to swell up and shrink again and it's happened a few times. Night sweats are also coming and going, where before they seemed to be starting to subside (never completely). Is this normal for the nodes and sweats to almost go away then come back and start to shrink and go away again?
I honestly won't be super optimistic till I see a new petscan which I guess won't happen till I've had a few cycles of ABVD. The doctors think that if I'm really improved they might dial back some of the harsher aspects of ABVD drugs to lower doses. My main concern after initial diagnosis (4B) was the Hodgkins in my vertebrae, spleen, etc. I can feel the nodes getting smaller (despite that one in my neck) and my Hodgkins symptoms (cough, no appetite, fatigue etc) have subsided, but I can't look inside myself to see if the spleen, vertebrae have gotten better.
Side effects from treatment have been pretty minor after the initial shock to the system. My beard thinned a lot. Body hair doesn't grow (I'm kind of happy about these lol- low maintence), fatigue is still major after chemo for about 4 days. I had horrible heartburn but never nausea. I'm taking prilosec for that now.
I agree with your overall sentiment that you are making progress, perhaps pretty good progress.
My hematologist and his group at our teaching hospital (about 25 oncologists) ordinarily doesn't do a progress CT until three full infusions are completed (all drugs scheduled administered 3 times). There are exceptions, but this is their general policy, so your doctor is similiar.
Nodes don't ordinarily "oscillate" up and down, at least not from Lymphoma, so I have no idea there. What will oscillate are hydration in the patient, etc.
Pulling for you and hope to hear good news in two weeks or so,
max
0 -
Thanks Max! Yeah I think IOverall
I agree with your overall sentiment that you are making progress, perhaps pretty good progress.
My hematologist and his group at our teaching hospital (about 25 oncologists) ordinarily doesn't do a progress CT until three full infusions are completed (all drugs scheduled administered 3 times). There are exceptions, but this is their general policy, so your doctor is similiar.
Nodes don't ordinarily "oscillate" up and down, at least not from Lymphoma, so I have no idea there. What will oscillate are hydration in the patient, etc.
Pulling for you and hope to hear good news in two weeks or so,
max
Thanks Max! Yeah I think I heard my oncologist/hematologist say they had to do 3 cycles first before another petscan. So I guess 4 more chemos (2 cycles) so I guess that means after Dec 15th. I'm going to basically put it out of my mind and try to not think about it at all.
The chemo curve was tough but usually 4-5 days (after chemo) I don't feel like a complete zombie. I'll be glad after the last Rituxan is done tomorrow because they dose me pretty hard with tylenol and benadryl prior to that and it knocks me out for 3 hrs in the chair. Guess that's a good thing to kill time, but it's never sleep sleep, more like out of it but still awake sleep.
0 -
Interesting
My oncologist ordered a Pet Scan for first week in December and I would only have received 2 cycles of ABVD and 6 Rituxan treatments. Guess he has high hopes- I on the other hand have to manage my expectations so I don't get disappointed.
That lymph node in my neck keeps shrinking and then getting bigger over an over so I suspect it's going to be a problem node they might eventually have to zap with radiation.
I try to be the half glass full kind of guy but I always seem to graviate towards half empty. Like yesterday all I could think of is what if none of this works, or works and I relapse? Hard not too even though I know I can't let that **** enter my mind.
0 -
Not sure how to take this news
So I had a interim pet scan on 12/7 and got my results today. Trying to be positive but it's hard. First let me say I've had 6 Rixtuxan treatments that started on 10/3 and ended 11/10. My ABVD chemo though has been erratic at best and perhaps that's why its not going as well as expected towards recovery. I've only had 2 cycles (4 treatments) because of infections and low ANC. So Chemo on 10/5, then 10/27 (delayed from 10/20), 11/10, then 12/1 (delayed from 11/24) and I'm due again this Friday 12/15 to start cycle 3.
So the first thing my doctor says to me is there has been nothing normal about your diagnosis or treatment, but there has been progress. There is no longer activity in my spleen, the osseous lesions appear to have gone in my vertebrae (or as the report puts it no definite involvement in osseous structures though sensitivity is decreased secondary to red marrow hypertrophy).
The rest of the report goes on to say slight interval decrease in size of multiple metabolically active lymph nodes, but markedly increased FDG avidity throughout lymph nodes, which has only slightly decreased since last study. Marked diffuse increased FDG uptake throughout red marrow likely related to treatment.
Here are some of the size differentials of lymph nodes in comparison to last time (with SUV maxes):
1) Neck: Active lymph nodes in left lower cervical into left supraclavical area- 3.5 x 3cm previously 3.9 x 3.4cm SUV max unchanged at 242) Chest: Unchanged 4mm pulmonary nodule in right upper lobe no increased FDG
3) Chest: Large active lymph nodes in left axilla and subpectoral- largest left axilla 4.2 x 4.1cm SUV max 30- was 5.9 x 5.4cm SUV max 35 previously. Largest subpectoral lymph node- 4.2 x 2.6cm SUV max 21, was 6.4 x 4.4cm SUV max 35
4) Abdomen and Pelvis: slightly increased prominence of top normal size periportal lymph nodes, slightly increased FDG avidity. Large mesenteric lymph node now measures 2.6 x 1.8cm with minimal FDG avidity, previously measuring 4.2 x 2.5cm SUV max 9.
Again I'm no doctor so I only can see slight decreases in node size /SUV. My doctor wants me to see a lymphoma specialist in the next month or two in Philadelphia but the colleague he suggested isn't in my Medicaid network I found out when I got home. For now he wants to stay the course and hopefully no more staph infections or low ANC and I can keep on this every two weeks ABVD schedule (I go again Friday).
So should I be hopeful? Like I said I wasn't expecting complete remission after 6 Rituxan and 2 cycles of ABVD but it sounds like the doctors were being overly optimistic (but won't admit it). I mean I was stage 4B NLPHL and now no activity in my bones or spleen and slightly shrunken lymph nodes (given my chemo has been erratic)- but FDG avidity is still strong.
0 -
Unsure AlsoLixx said:Not sure how to take this news
So I had a interim pet scan on 12/7 and got my results today. Trying to be positive but it's hard. First let me say I've had 6 Rixtuxan treatments that started on 10/3 and ended 11/10. My ABVD chemo though has been erratic at best and perhaps that's why its not going as well as expected towards recovery. I've only had 2 cycles (4 treatments) because of infections and low ANC. So Chemo on 10/5, then 10/27 (delayed from 10/20), 11/10, then 12/1 (delayed from 11/24) and I'm due again this Friday 12/15 to start cycle 3.
So the first thing my doctor says to me is there has been nothing normal about your diagnosis or treatment, but there has been progress. There is no longer activity in my spleen, the osseous lesions appear to have gone in my vertebrae (or as the report puts it no definite involvement in osseous structures though sensitivity is decreased secondary to red marrow hypertrophy).
The rest of the report goes on to say slight interval decrease in size of multiple metabolically active lymph nodes, but markedly increased FDG avidity throughout lymph nodes, which has only slightly decreased since last study. Marked diffuse increased FDG uptake throughout red marrow likely related to treatment.
Here are some of the size differentials of lymph nodes in comparison to last time (with SUV maxes):
1) Neck: Active lymph nodes in left lower cervical into left supraclavical area- 3.5 x 3cm previously 3.9 x 3.4cm SUV max unchanged at 242) Chest: Unchanged 4mm pulmonary nodule in right upper lobe no increased FDG
3) Chest: Large active lymph nodes in left axilla and subpectoral- largest left axilla 4.2 x 4.1cm SUV max 30- was 5.9 x 5.4cm SUV max 35 previously. Largest subpectoral lymph node- 4.2 x 2.6cm SUV max 21, was 6.4 x 4.4cm SUV max 35
4) Abdomen and Pelvis: slightly increased prominence of top normal size periportal lymph nodes, slightly increased FDG avidity. Large mesenteric lymph node now measures 2.6 x 1.8cm with minimal FDG avidity, previously measuring 4.2 x 2.5cm SUV max 9.
Again I'm no doctor so I only can see slight decreases in node size /SUV. My doctor wants me to see a lymphoma specialist in the next month or two in Philadelphia but the colleague he suggested isn't in my Medicaid network I found out when I got home. For now he wants to stay the course and hopefully no more staph infections or low ANC and I can keep on this every two weeks ABVD schedule (I go again Friday).
So should I be hopeful? Like I said I wasn't expecting complete remission after 6 Rituxan and 2 cycles of ABVD but it sounds like the doctors were being overly optimistic (but won't admit it). I mean I was stage 4B NLPHL and now no activity in my bones or spleen and slightly shrunken lymph nodes (given my chemo has been erratic)- but FDG avidity is still strong.
When I got my PETS back in 2009, the hematologist never mentioned FDG or SUV. But my progress in treatment was not problematic. All he ever referenced (to me) was node size. A few people here in the last year have written about SUV, but I am not sure how much to make of it.
What I find most negative in your report is that your doctor "wants you to see a Lymphoma specialist." By all means ! Lymphoma is at its worst when first-line treatment stalls. Things become infinitely more complex, fast. If I couldn't do a consult witht he doctor recommended by your doctor, I would nonetheless see someone for a review.
Progress is progress, and at least early in you have experienced across the board size reductions among the nodes. Ordinarily NLPHL is easily put in to full remission with little resistance. If it is being resistant (which is unclear at this point), it may be because other things are going on. As I wrote to you when we first met, correct pathology/diagnosis is fundamental.
max
0
Discussion Boards
- All Discussion Boards
- 6 CSN Information
- 6 Welcome to CSN
- 122.1K Cancer specific
- 2.8K Anal Cancer
- 448 Bladder Cancer
- 309 Bone Cancers
- 1.6K Brain Cancer
- 28.5K Breast Cancer
- 398 Childhood Cancers
- 27.9K Colorectal Cancer
- 4.6K Esophageal Cancer
- 1.2K Gynecological Cancers (other than ovarian and uterine)
- 13K Head and Neck Cancer
- 6.4K Kidney Cancer
- 673 Leukemia
- 795 Liver Cancer
- 4.1K Lung Cancer
- 5.1K Lymphoma (Hodgkin and Non-Hodgkin)
- 239 Multiple Myeloma
- 7.2K Ovarian Cancer
- 65 Pancreatic Cancer
- 490 Peritoneal Cancer
- 5.5K Prostate Cancer
- 1.2K Rare and Other Cancers
- 543 Sarcoma
- 738 Skin Cancer
- 658 Stomach Cancer
- 192 Testicular Cancer
- 1.5K Thyroid Cancer
- 5.9K Uterine/Endometrial Cancer
- 6.3K Lifestyle Discussion Boards