Another person diagnosed with NLPHL
Hello everyone,
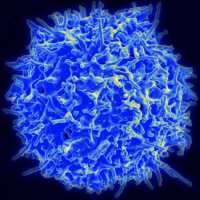
Former lurker here. It seems like only a small number people on this forum have had NLPHL, but it looks like you can add me to the list. I am a 32 year old male, went to urgent care with a cold 5 months ago and they did a chest X-Ray and found something that looks like scarring in my lung. That then lead to a CT scan and the scarring is still a mystery, but they discovered that I had several enlarged inguinal lymph nodes on two lymph systems in my left side (max 4cm dia.). I remember noticing this lump in my leg a few months earlier, but I thought it might just be a new muscle I was developing from my new hobby of skateboarding. I have no B symptoms.Two weeks ago I had an excisional biopsy of the largest lymphnode, and a few days ago the pathology came in with a NLPHL diagnosis. My atypical cells were positive for: Bob1, CD19, CD20, EMA, CD45 (LCA), Oct2, and Pax5. The bad cells were rimmed by CD57s.
I finally have a diagnosis--which honestly was a bit of a relief, I was not thrilled with looking at the mystery lump every day for 5 months. Now I have a CT, PET, and bone marrow biopsy lined up for staging. With the data as they are right now, my Onc. thinks I will only need radiation treatments 5 days a week for a month, no chemo. I expect he will give me more detail as the staging becomes more clear. This seems to go against what others have reported here in the forum; with many that have NLPHL getting some sort of chemo treatment.
My Onc. assures me that I am somewhat lucky to get NLPHL over other types of lymphoma. My thinking is in line with others on this forum in that I feel lucky to have something that is likely to be curable, but it is hard to convince myself that everything will be fine in just a few short months. The fact that I have two young kids makes things a bit difficult too.
Anyway, just figured I would introduce myself. I'll be posting updates as they come. Any advice would be appreciated.
Comments
-
Many choices, one hope
Sorry to welcome you here. Even though NLPHL is called a form of Hodgkin's, it seems to be either a rare variation of indolent B-Cell Lymphomas, or perhaps its own entity. It exhibits a lot of differences from the various Hodgkin's Lymphomas. Radiation is an acceptable treatment by itself, depending on individual circumstances. Chemotherapy may be morphing from the old-school ABVD regimen into R-CHOP, as the disease seems to respond failrly well to it. The problem is, that among all of the other uncertainlies involved, the proper treatment in your case can also be up in the air. There are many factors which your hematologist will have to weigh in order to arrive at what is essentially a judgment call. Sadly, that is the cancer world.
There is good reason to consider R-CHOP rather than the lung-toxic ABVD. There is reason to use radiation alone. There is reason to use a radiation/chemo combination - the field is changing rapidly as the disease is becoming better understood. The good news in all of this is that relapsed disease - very common with indolent B-Cell Lymphomas - responds well to subsequent therapy - something that cannot be said for all forms of Hodgkin's Lymphoma.
I would suggest, at the very minimum, a consult with a NLPHL specialist at a major cancer center or research facility. You want the latest and greatest treatment, as well as the best and brightest hematologist on your case. Consider being treated at such a facility, as outcomes are simply better there. They are immersed in research and thus possess the latest intellegence regarding treatment. Travel if you must, as treatment will not last forever.
Max will chime in soon. He is the resident expert on all things NLPHL.
0 -
po18guy said:
Many choices, one hope
Sorry to welcome you here. Even though NLPHL is called a form of Hodgkin's, it seems to be either a rare variation of indolent B-Cell Lymphomas, or perhaps its own entity. It exhibits a lot of differences from the various Hodgkin's Lymphomas. Radiation is an acceptable treatment by itself, depending on individual circumstances. Chemotherapy may be morphing from the old-school ABVD regimen into R-CHOP, as the disease seems to respond failrly well to it. The problem is, that among all of the other uncertainlies involved, the proper treatment in your case can also be up in the air. There are many factors which your hematologist will have to weigh in order to arrive at what is essentially a judgment call. Sadly, that is the cancer world.
There is good reason to consider R-CHOP rather than the lung-toxic ABVD. There is reason to use radiation alone. There is reason to use a radiation/chemo combination - the field is changing rapidly as the disease is becoming better understood. The good news in all of this is that relapsed disease - very common with indolent B-Cell Lymphomas - responds well to subsequent therapy - something that cannot be said for all forms of Hodgkin's Lymphoma.
I would suggest, at the very minimum, a consult with a NLPHL specialist at a major cancer center or research facility. You want the latest and greatest treatment, as well as the best and brightest hematologist on your case. Consider being treated at such a facility, as outcomes are simply better there. They are immersed in research and thus possess the latest intellegence regarding treatment. Travel if you must, as treatment will not last forever.
Max will chime in soon. He is the resident expert on all things NLPHL.
Thank you sir for your kind welcome, and your advice to go to a major cancer center. Fortunately, I am being seen at a research hospital, the University of California, San Diego -- Moores Cancer Center. Although it is not necessarily one of the storied cancer research facilities (e.g., MD Anderson), I suspect it ranks somewhere between the storied centers and your average local hospital. My current Onc. is blood cancer specialist, but he said that he has treated several NLPHL cases, roughly once every year or two when one of us rare birds comes knocking. Once I have my staging results, I plan on running the treatment plan by at least one more doctor to see if they agree with going radiation only over anything involving chemo.
I see what you mean by there not being one true answer. More than anything in my life, being diagnosed with cancer has made me realize that we exist in a world of uncertainty. Unfortunately, the dice rolls were not in my favor in that I won't be making it out out of my 30s without a cancer diagnosis, but it seems like they are in my favor in that NLPHL is one of the more treatable types of cancer one can have.
One other question I have is, what effect will this will have on my work? I am a teacher, and I am slated to start teaching a few days after my staging tests end. My gut says I might be able to continue teaching as if nothing is happening, but I don't trust my instinct because the only thing I know about the future is that my Onc. is leaning toward a radiation-only treatment plan. I do have a standing offer from some of my colleagues to take over my class until the treatment is over. That certainly would make my life much easier, but handing over the responsibility is likely to severely inconvenience them.
0 -
NLPHL club
Well this is a club no one wanted to join. I had this as well as Non Hodgkins at the same time. I was on RCHOP for 6 treatments. Not sure how it goes with radiation because never had that. In answer to working. I can only speak to Chemo . I am 53 and I had lost 41 pounds before diagnosis and treatment began. The first 3 treatments I could have probably forced myself to work and not been unbearable except for the 8th day after infusion when I crashed from coming off Prednisone after 5 days. Treatment 4 would have been much harder and 5 and 6 I was really fatigued. Could I have forced myself? Maybe but the fatigue was something like I had never experienced and it took about 4 weeks to finally get to feeling good again. I cannot explain to people who have not had Chemo how the fatigue makes you feel. It is not just being tired. On a positive note it was temporary. I now feel fine just lost all muscle so cannot do a lot of manual labor type stuff. I think that will come back as well.
The side effects for me other than fatigue were not unbearable. This forum and people on it helped me figure out some things to help with those side effects. Lost my hair, my muscle but never my sense of humor. Worst part for me was just looking sick all the time like I was taking Chemo . Yeah I was but I just wanted to look like an average Joe out and about in public . If you end up getting Chemo many on here will be willing to help with suggestions.
So bottom line is. This is not fun! It is beatable. It has and will change how you view life. I would let your friends help when you start feeling the fatigue. I mowed my grass all but maybe 2-4 times this summer. However on treatments 5 and 6 I just finally let someone help. They were willing and it was what they could do to show they cared. I saved my energy to help me make it through the day. I only worked maybe 10 days during all 6 treatments so almost 5 months. Luckily I had a job I could do that .
I have been done with last treatment 9 weeks now. Appetite back with a vengeance. Had Pet scan Friday get new results Tuesday. Never went to doctors much before. Life has changed but it is still good.
Richard is our expert so I am sure he will chime in soon.
Please do not disappear from the forum. Let us know how things are going.
Praying your journey is good.
Sandy
0 -
Happy to join the crew
Hi Sandy, thanks for sharing your experience. I have also noticed that humor is a key tool to making it through this process. When I was informing folks of my diagnosis I told them something like, "I have cancer, but it's the kind of cancer that everyone dreams of!"
Based on your comments and what I have heard from others, if my Dr. advises that I need chemo I will immeadiatly take up the offer to have my colleages take over my class. As you said, I want to make sure I use my energy wisely while I have a cocktail of magical chemicals storming their way through my body. If anyone has experienced the radaition therpy (e.g., ISRT)-- or "The Big Zap" as I have been calling it--I would be interested to hear how that affected your ability to continue your normal daily family/work life.
I actually have another medical condition, so fortunately this is not my first time at the hospital rodeo. A few years ago I activated Ulcerative Colitis in my body when I got a nasty parasite in Guatemala. NLPHL sounds scarier on paper, but at least there are known treatments that can get you into remision. Getting UC into remission is very much a cat-and-mouse-game.
I will be sure to keep you all up to date. Next step is the CT scan on Tuesday.
Let's do this.
0 -
Immune suppression potentialskaterdad said:Thank you sir for your kind welcome, and your advice to go to a major cancer center. Fortunately, I am being seen at a research hospital, the University of California, San Diego -- Moores Cancer Center. Although it is not necessarily one of the storied cancer research facilities (e.g., MD Anderson), I suspect it ranks somewhere between the storied centers and your average local hospital. My current Onc. is blood cancer specialist, but he said that he has treated several NLPHL cases, roughly once every year or two when one of us rare birds comes knocking. Once I have my staging results, I plan on running the treatment plan by at least one more doctor to see if they agree with going radiation only over anything involving chemo.
I see what you mean by there not being one true answer. More than anything in my life, being diagnosed with cancer has made me realize that we exist in a world of uncertainty. Unfortunately, the dice rolls were not in my favor in that I won't be making it out out of my 30s without a cancer diagnosis, but it seems like they are in my favor in that NLPHL is one of the more treatable types of cancer one can have.
One other question I have is, what effect will this will have on my work? I am a teacher, and I am slated to start teaching a few days after my staging tests end. My gut says I might be able to continue teaching as if nothing is happening, but I don't trust my instinct because the only thing I know about the future is that my Onc. is leaning toward a radiation-only treatment plan. I do have a standing offer from some of my colleagues to take over my class until the treatment is over. That certainly would make my life much easier, but handing over the responsibility is likely to severely inconvenience them.
As school starts, so also begins the cold and flu season. You might pointedly ask doctor about any immune suppression that you will experience as a result of treatment. Infections that are annoyances can become serious threats if your immune system is compromised by treatment. My last "common cold" (Rhinovirus) lasted 3 months due to my immune suppression. Along with it came two months of Human Respiratory Syncytial Virus and pneumoniua in my left lung. February through May essentially evaporated as I fought the infections.
0 -
Welcomeskaterdad said:Thank you sir for your kind welcome, and your advice to go to a major cancer center. Fortunately, I am being seen at a research hospital, the University of California, San Diego -- Moores Cancer Center. Although it is not necessarily one of the storied cancer research facilities (e.g., MD Anderson), I suspect it ranks somewhere between the storied centers and your average local hospital. My current Onc. is blood cancer specialist, but he said that he has treated several NLPHL cases, roughly once every year or two when one of us rare birds comes knocking. Once I have my staging results, I plan on running the treatment plan by at least one more doctor to see if they agree with going radiation only over anything involving chemo.
I see what you mean by there not being one true answer. More than anything in my life, being diagnosed with cancer has made me realize that we exist in a world of uncertainty. Unfortunately, the dice rolls were not in my favor in that I won't be making it out out of my 30s without a cancer diagnosis, but it seems like they are in my favor in that NLPHL is one of the more treatable types of cancer one can have.
One other question I have is, what effect will this will have on my work? I am a teacher, and I am slated to start teaching a few days after my staging tests end. My gut says I might be able to continue teaching as if nothing is happening, but I don't trust my instinct because the only thing I know about the future is that my Onc. is leaning toward a radiation-only treatment plan. I do have a standing offer from some of my colleagues to take over my class until the treatment is over. That certainly would make my life much easier, but handing over the responsibility is likely to severely inconvenience them.
I have never received therapeudic radiation, skater, but most of my Prostate cancer buddies (my other cancer) have. A little radiation ordinarily doesn't involve any disability or imparement at all for them. Sometimes, a little fatigue. Nothing like chemo, as you have suggested.
NLPHL Stage 1 or 2 is fairy routinely treated with radiation alone, or radiation with a dinky dab of R-ABVD, a few infusions. My guess is that you are Stage 2. But Stage 4 Lymphomas are not a lot harder to eradicate than a Stage 2. The fact that NLPHL expresses (as you did) CD-20 is why Rituxan is included with ABVD. No other form of Hodgkin's has CD-20, and no other form of Hodgkin's therefore uses Rituxan in its treatment. NLPHL is easily put into full remission, but has some tendency to reappear, like most indolent (non-aggressive) Lymphomas; the rate for this is around 15%, but complete remission will frequently last 10 years or more, even for them. And a 15% relapse rate means an 85% rate of NOT relapsing.
If you receive radiation only, I cannot imagine not being able to do any job, with no one noticing at all. Many writers here have worked full time during even high-dose R-CHOP or other harsh programs. Going for radiation is much easier than an afternoon at the beach. A visit at my oncology center for radiation is less than an hour, but for a person in Charleston to go to the beach is a day-long ordeal. Look at it that way. I was never more miserable in my life than when taking the kids to Disney World in Orlando. An hour wait for every ride; endless mobs of pushy, thoughtless people. Everyone at the radiation center whill have recently bathed, and not smell. NOT SO at Disney World.
The impairement and weakness of people with Lymphoma is frequently more attributable to the treatments, rather than the disease itself. But the treatments are of course essential. I'd rather have side-effects than have cancer.
max
0 -
ha!Welcome
I have never received therapeudic radiation, skater, but most of my Prostate cancer buddies (my other cancer) have. A little radiation ordinarily doesn't involve any disability or imparement at all for them. Sometimes, a little fatigue. Nothing like chemo, as you have suggested.
NLPHL Stage 1 or 2 is fairy routinely treated with radiation alone, or radiation with a dinky dab of R-ABVD, a few infusions. My guess is that you are Stage 2. But Stage 4 Lymphomas are not a lot harder to eradicate than a Stage 2. The fact that NLPHL expresses (as you did) CD-20 is why Rituxan is included with ABVD. No other form of Hodgkin's has CD-20, and no other form of Hodgkin's therefore uses Rituxan in its treatment. NLPHL is easily put into full remission, but has some tendency to reappear, like most indolent (non-aggressive) Lymphomas; the rate for this is around 15%, but complete remission will frequently last 10 years or more, even for them. And a 15% relapse rate means an 85% rate of NOT relapsing.
If you receive radiation only, I cannot imagine not being able to do any job, with no one noticing at all. Many writers here have worked full time during even high-dose R-CHOP or other harsh programs. Going for radiation is much easier than an afternoon at the beach. A visit at my oncology center for radiation is less than an hour, but for a person in Charleston to go to the beach is a day-long ordeal. Look at it that way. I was never more miserable in my life than when taking the kids to Disney World in Orlando. An hour wait for every ride; endless mobs of pushy, thoughtless people. Everyone at the radiation center whill have recently bathed, and not smell. NOT SO at Disney World.
The impairement and weakness of people with Lymphoma is frequently more attributable to the treatments, rather than the disease itself. But the treatments are of course essential. I'd rather have side-effects than have cancer.
max
Hillarious. Living in San Diego, I can totally relate to the day-long ordeal that is going to the beach. Thanks for the positive vibes
 0
0 -
SandySandy Ray said:NLPHL club
Well this is a club no one wanted to join. I had this as well as Non Hodgkins at the same time. I was on RCHOP for 6 treatments. Not sure how it goes with radiation because never had that. In answer to working. I can only speak to Chemo . I am 53 and I had lost 41 pounds before diagnosis and treatment began. The first 3 treatments I could have probably forced myself to work and not been unbearable except for the 8th day after infusion when I crashed from coming off Prednisone after 5 days. Treatment 4 would have been much harder and 5 and 6 I was really fatigued. Could I have forced myself? Maybe but the fatigue was something like I had never experienced and it took about 4 weeks to finally get to feeling good again. I cannot explain to people who have not had Chemo how the fatigue makes you feel. It is not just being tired. On a positive note it was temporary. I now feel fine just lost all muscle so cannot do a lot of manual labor type stuff. I think that will come back as well.
The side effects for me other than fatigue were not unbearable. This forum and people on it helped me figure out some things to help with those side effects. Lost my hair, my muscle but never my sense of humor. Worst part for me was just looking sick all the time like I was taking Chemo . Yeah I was but I just wanted to look like an average Joe out and about in public . If you end up getting Chemo many on here will be willing to help with suggestions.
So bottom line is. This is not fun! It is beatable. It has and will change how you view life. I would let your friends help when you start feeling the fatigue. I mowed my grass all but maybe 2-4 times this summer. However on treatments 5 and 6 I just finally let someone help. They were willing and it was what they could do to show they cared. I saved my energy to help me make it through the day. I only worked maybe 10 days during all 6 treatments so almost 5 months. Luckily I had a job I could do that .
I have been done with last treatment 9 weeks now. Appetite back with a vengeance. Had Pet scan Friday get new results Tuesday. Never went to doctors much before. Life has changed but it is still good.
Richard is our expert so I am sure he will chime in soon.
Please do not disappear from the forum. Let us know how things are going.
Praying your journey is good.
Sandy
Who is Richard, the expert?
Wondering,
Rocquie
0 -
"Once every year or two"?
I would hope that he is 1) a researcher or 2) readily and willingly consults with a NLPHL researcher, as progress has been and is being made as we speakagainst NLPHL. I live in a different lymphoma world, but the new-at-the-time salvage regimen which put me in my pre-transplant remission in 2015 is now outdated! There is better out there than the age-old ABVD. Perhaps there is even a newer, better regimen than R-CHOP. Seriously look into a clinical trial, as you can receive cutting edge drugs years before they hit the market. And, if the trial drugis not effective in your case, standard therapy can quickly be put in place. I have now participated in three clinincal trials - two for lymphoma and one for chronic Graft Versus Host Disease. The first trial placed me in full response after an immediate relapse and kept me there for 4 1/2 years, which is forever in the T-Cell world.
0 -
Indeedpo18guy said:"Once every year or two"?
I would hope that he is 1) a researcher or 2) readily and willingly consults with a NLPHL researcher, as progress has been and is being made as we speakagainst NLPHL. I live in a different lymphoma world, but the new-at-the-time salvage regimen which put me in my pre-transplant remission in 2015 is now outdated! There is better out there than the age-old ABVD. Perhaps there is even a newer, better regimen than R-CHOP. Seriously look into a clinical trial, as you can receive cutting edge drugs years before they hit the market. And, if the trial drugis not effective in your case, standard therapy can quickly be put in place. I have now participated in three clinincal trials - two for lymphoma and one for chronic Graft Versus Host Disease. The first trial placed me in full response after an immediate relapse and kept me there for 4 1/2 years, which is forever in the T-Cell world.
Very good point Po: A doc who sees a disease a few times a decade is not exactly "proficient," in most cases. It also suggests a smallish practice. And stuff does happen fast in treatment development. I recall when the treatment Becky found for Bill was cutting edge; I believe she had to speak to German researchers to learn abou it, but today, there are newer approaches to MCL.
Skater: Upon re-reading, I view my post above regarding radiation therapy as a bit too "walk in the park," altough what I wrote is accurate: Radiation is usually easy to get, with (usually) few side effects. There is the rare burn injury to an adjacent organ, but radiation today is extremely precise in delivery. As with chemo, there have been dramatic advances in radiation oncology in the last ten year or so.
I want to also add that I (as a layperson with no training) have never been comfortable with the notion of just radiation for any blood disease, although it is employed (successfully) by some doctors against early-stage Lymphoma. Lymphoma is systemic,-- potentially everywhere -- not just in spots visible on PET or CT. I have read more than one report that recommeded some chemo be included against early stage disease, even if radiation is primary. The results of those studies indicated better long-term cure than radiation applied alone.
Radiation is what the SCT Director at my cancer center calls "spot welding": It can kill a node or other tumor, but not a lot else, even when applied as a "field." Often, radiation is the only choice in tumors inaccessable to surgery, as in common in the brain. But radiation with chemo increases later chances of developing a treatment-induced leukemia, verses chemo by itself (some chemos alone have leukemia-inducing potential alone). This likelihood of getting leukemia is extremely small either way, but it does exist.
When I was diagnosed with prostate cancer ("PCa") I had the option of either radiation by itself or surgery by itself. It was a flip of the coin for cure, since both, for first-line, non-metastatic PCa are equally curative. RT has many fewer side-effects than PCa surgery, but I chose surgery anyway. I just did not want the toxicity of heavy radiation added to my treatment history. So there are an assortment of trade-offs to ask your doctors about.
If I ever relapsed with any strain of Lymphomma, even if it were only a single detectable node, I would refuse radiation myself and go with second-line chemo. Just me, and an opinion I have held for nearly a decade now. I have not intended to muddy the water. Again, you need a best practices doctor, as Po suggested. "The money" has not lead to a huge amount of NLPHL research, since the disease is so rare, but there has been some. I hope your doctor has read all of it,
max
0 -
Max and p018guy. Thank you
Max and p018guy. Thank you very much for your replies. I do want to make sure my primary onc, or at least an onc I am consulting with, is well read on NLPHL. However, is it reasononable to expect that any onc sees more than one or two cases of NLPHL per year given how rare the diagnosis is?
Once I get staged and my onc gives me a treatment plan (CT today, yay!), my plan is to consull with any NLPHL experts that I can find. I suspect that there will be at least one in southern california. If not, I am even happy to fly somewhere to consult with an expert (Austin here we come!). My goal is to pick the best treatment plan, get this thing taken care of, and move on with my life.
When you all were going through your respective treatments for NLPHL, how did you find an onc who was an expert in NLPHL to handle your case?
0 -
NLPHL carries the potential to transform into aggressive DLBCL
I am certain that you want to avoid this if at all possible. As opposed to the T-Cell Lymphoma world, NLPHL is fairly common. Really. Still, you want someone who knows it intimately. You want a doctor who hates it. One who will take your case file home, if that is what it requires. This will probably require Googling and traveling. NLPHL is indolent, which gives you the blessing of time. Still, if you can put it into remission for an extended period, that is far better, as many new treatments and knowledge of the lymphoma will have advanced by that time. I am huge on seeking out the best of the best - no matter your type or sub-type. Being providentially directed to one of the world's best T-Cell specialists has saved my life at least three times.
0 -
Found the Report
skater,
I found one of the studies that I had mentioned somewhere above, that indicates that Radiation with accompanying R-ABVD is much more effective in ensuring long-term freedom from relapse in NLPHL, verses RT alone.
While RT (Radiation Therapy) for Stage 1 or 2 is nearly 100 effective in ensuring Complete Remission (CR) of NLPHL, the previous studies were looking at only 5 years post-treatment. With a few cycles of R-ABVD added, the freedom from relapse (FFTF -- 'freedom from treatment failure') doubled (i.e., long-term relapse happened less than half as often). Two cycles (4 infusions) of R-ABVD is not ordinarily very toxic, since toxicity builds with total dose, and toxicity is for some reason usually linked to older patients. I did 12 infusions covering 6 months and was 53 at the time. My experience was quite harsh, but I both had a lot of the drugs, and was older than the norm.
Po is correct that there may be less toxic combinations for NLPHL than R-ABVD, but R-ABVD was itself created to reduce the toxicity of what was used before that for NLPHL, a combination known as MOPP. MOPP is still used occasionally today, but is quite rare. And Rituxan was not used with ABVD until relatively recent times. Prior to that, doctors were relatively complacent in using just ABVD, thinking that if NLPHL were simply an oddball HL, Rituxan was irrelevant. Studies proved that notion very wrong.
The summary of the study is in Table 1. I would print and provide that study Abstract to your doctor and ask his opinion. The journal Blood is one of the most highly regarded in the hematology realm. While the report is over 4 years old, as I noted, not that much is being done on this strain, compared to the more popular Lymphomas.
Radiation alone WILL ordinarily put early-stage NLPHL into full remission; all agree on that. The question is, for how long ? This one study suggests with a little R-ABVD, around twice as long.
One other point of agreement with Po I want to repeat: NLPHL is slow-moving, non-aggressive. It is a lazy disease. Take your time choosing a doctor, since there is absolutely no rush. Some oncologists even use Active Survellance with NLPHL, but I am not a fan, and could never be comfortable with A/S myself against any form of cancer. And I also want to repeat that your current oncologist might be a great guy and very conversant, even regarding NLPHL. But I would ask !
max
http://www.bloodjournal.org/content/122/26/4288?sso-checked=true
0 -
Post CT, going forward
Thanks again po18guy and Max for the additional information. You all must be seers, because I just got my CT results back and it looks like I have mild (14cm) splenomegaly as well as the enlarged lyph nodes in 3 systems on my left side below the diaphragm on my left side. This means that the information you have provided is beocming increasingly relevant, especially because splenic involvment increases the chances of transformation into DLBCL.
The good news is they have reported no other new lymph node involvement, just the spleen!
I also suppose that means i am going to be categorized as at least Stage III at this point. That is unless there is another good reason why my spleen has grown in size. From what I have read, it sounds like NLPHL is the likely cause. This also means I am likely to be on the Chemo train rather than the radiation train, woo woo!
In an abudance of caution, and following po18guy's advice, I made an appointment at MD Anderson for the middle of October with their apparent NLPHL expert. Michelle A. Fanle. The good news is I managed to buy flights from San Diego to Houston for $100 - *round trip* (thanks Southwest!).
With all bad news comes some good news, I guess this is the way forward with the Big Casino.
0 -
Considerskaterdad said:Post CT, going forward
Thanks again po18guy and Max for the additional information. You all must be seers, because I just got my CT results back and it looks like I have mild (14cm) splenomegaly as well as the enlarged lyph nodes in 3 systems on my left side below the diaphragm on my left side. This means that the information you have provided is beocming increasingly relevant, especially because splenic involvment increases the chances of transformation into DLBCL.
The good news is they have reported no other new lymph node involvement, just the spleen!
I also suppose that means i am going to be categorized as at least Stage III at this point. That is unless there is another good reason why my spleen has grown in size. From what I have read, it sounds like NLPHL is the likely cause. This also means I am likely to be on the Chemo train rather than the radiation train, woo woo!
In an abudance of caution, and following po18guy's advice, I made an appointment at MD Anderson for the middle of October with their apparent NLPHL expert. Michelle A. Fanle. The good news is I managed to buy flights from San Diego to Houston for $100 - *round trip* (thanks Southwest!).
With all bad news comes some good news, I guess this is the way forward with the Big Casino.
Ask the doctor is splenectomy is advisible in your case. Usually not necessay, but there are situations when it is. Not recommending, just saying "ask."
The questions are free at MDA and elsewhere (they are part of the $10 K consult
 ).0
).0 -
Anemia?
I didn't see reference to it, but are you anemic? Spleen enlargement goes hand in hand with anemia, as the spleen sucks up red blood cells. I had moderate splenomegaly, but it was most likely caused by the cytokines released by the tumor cells. Normally, it is: Kill the tumors, kill the spleen enlargement.
0 -
PET scan results
Hello everybody,
So the PET scan results are in (drumroll...). As expected, my left external iliac and inguinal lymph nodes lit up, but also so did nodes in right axiliary and aortocaval and mesenteric lymph systems. Also my spleen lit up more than my liver, so they think that's involved too. Needless to say, we are now above and below the diaphram! So much for easy-peesy stage one NLPHL

My primary Onc. now suggests 6 rounds of R-CHOP. Also he immediately scheduled me to meet with the top Lymphoma specialist at UC San Diego. Needless to say, on Monday I am planning on calling MD Anderson to see if I can move up my Oct 16 appointment as soon as possible. Anyone have any experience convincing the MD Anderson folks to get an appointment sooner than they initially said were available?
0 -
"ASAP"skaterdad said:PET scan results
Hello everybody,
So the PET scan results are in (drumroll...). As expected, my left external iliac and inguinal lymph nodes lit up, but also so did nodes in right axiliary and aortocaval and mesenteric lymph systems. Also my spleen lit up more than my liver, so they think that's involved too. Needless to say, we are now above and below the diaphram! So much for easy-peesy stage one NLPHL

My primary Onc. now suggests 6 rounds of R-CHOP. Also he immediately scheduled me to meet with the top Lymphoma specialist at UC San Diego. Needless to say, on Monday I am planning on calling MD Anderson to see if I can move up my Oct 16 appointment as soon as possible. Anyone have any experience convincing the MD Anderson folks to get an appointment sooner than they initially said were available?
Skater,
Can't tell for sure about MDA's policy regarding bumping up appointments, but in my experience sending your test results to the doctor you need to see will get them to decide that you need to be seen at an earlier date.
Do not worry too much about it though - as it is now clear that, whatever hospital you turn to for treatment, you will be getting chemotherapy, I would read "ASAP" as "in a couple of weeks (at least), once your cardiac function test is done and you have been fitted with a port"...
So, I believe you can get those preliminary tests and get the port surgery done while waiting for your second opinion appointment even if it is still in three weeks. Then, whether you decide to go with MDA or stay with UC San Diego, there will be no further delay before treatment is initiated.
Hope all goes well. Do keep us posted!
PBL
0 -
MD Anderson
Hey Skaterdad,
Yes my last PET scan showed activity. My Oncologist wanted me to go back to MD Anderson since activity was spleen and my spleen is still enlarged from original diagnosis. They originally scheduled for 10/20/2017. I sent the Dr an email and they rescheduled for 10/12 and would have been sooner but that is his first day back from vacatIon. Just let them know you want a second opinion and your Oncologist is wanting to start treatments asap! However, having the port in a week or two is good before first treatment. Will give it a little while for swelling to go down before they access it. Also this type of Lymphoma is usually indolent so not super big hurry.
I had 6 rounds of RCHOP as well. It is not fun but also not unbearable. Stay on the forum and you will have lots of people here to help you through.
Praying things go well for you.
Sandy Ray
0
Discussion Boards
- All Discussion Boards
- 6 CSN Information
- 6 Welcome to CSN
- 122.1K Cancer specific
- 2.8K Anal Cancer
- 448 Bladder Cancer
- 309 Bone Cancers
- 1.6K Brain Cancer
- 28.5K Breast Cancer
- 398 Childhood Cancers
- 27.9K Colorectal Cancer
- 4.6K Esophageal Cancer
- 1.2K Gynecological Cancers (other than ovarian and uterine)
- 13K Head and Neck Cancer
- 6.4K Kidney Cancer
- 673 Leukemia
- 795 Liver Cancer
- 4.1K Lung Cancer
- 5.1K Lymphoma (Hodgkin and Non-Hodgkin)
- 239 Multiple Myeloma
- 7.2K Ovarian Cancer
- 65 Pancreatic Cancer
- 490 Peritoneal Cancer
- 5.5K Prostate Cancer
- 1.2K Rare and Other Cancers
- 543 Sarcoma
- 738 Skin Cancer
- 658 Stomach Cancer
- 192 Testicular Cancer
- 1.5K Thyroid Cancer
- 5.9K Uterine/Endometrial Cancer
- 6.3K Lifestyle Discussion Boards