URGENT! Help please!!! Relapsed/Refractory NHL ALK+ ALCL

My husband is 23 years old. He is active duty military, we have two boys ages 4 & 6 years old. He was diagnosed with stage 4 anaplastic large t cell lymphoma alk + last October 2016. He started CHOEP, did 6 rounds and showed great response. Unfortunately 4 weeks later after his last treatment, he relapsed. He started brentuximab and a few rounds of intrathecal chemo which brought him into a remission again for an AUTO stem cell transplant and CD30 CAR T trial here at UNC in NC. He had a PET scan June 13th which showed he was in remission still and good for transplant. He had his transplant June 20th. He started having light night sweats and stomach pain. Doctors shrugged it off and said it was most likely due to the transplant. He had the CAR T infusion on July 11th and spiked a fever a few days later. We have been in the hospital since July 15th again. Doctors were hoping the fever were just CRS and a sign that the CAR T cells were doing their job. He had a PET scan two weeks ago that showed some hot spots but doctors said they weren't really concerned because they thought it was just the CAR T cells. Hes had high fevers for 2.5 weeks now, ranging between 103-105 degrees, drenching night sweats and horrible stomach pain. They just did another PET scan 2 days ago and have declared the AUTO stem cell transplant and CAR T trial a failure. The PET scan showed disease progression. This is my husbands 3rd time battling this monster in these past 10 months. The PET revealed uptake in the abdomen, a mass in his right calf which is where the relapse was the second time and left axillary lymph node which is where original diagnosis began. He has uptake around aorta, his back, left testicle which is very swollen and tender, chest wall, left tonsil and ribs.
They started him on brentuximab and steroids a few days ago and are not sure what to do at this point. They are saying the prognosis is pretty grim and we refuse to believe that. His fevers have subsided since they started the brentuximab and steroids, his stomach pain is gone, just has a little bit of discomfort still. His right calf is still aching where the mass is and his testicles are still sore and tender as well. However, they dont believe there is a mass in the testicles, just buildup of a lot of fluid.
Does anyone have suggestions? We are hoping to get down to MD Anderson within the next two weeks, just waiting on insurance approval.
Who has had this exact disease and has anyone relapsed this many times in such a short period? What chemo/anything has helped get you into a remission? We need some hope. We are willing to try and do anything. Please help our family!
Comments
-
You might consider New York or Seattle (SCCA/Fred Hutchinson)
I know that MD Anderson is a world-class facility, and they may have a T-Cell specialist there, but I am not familiar with one. I do know thart Dr. Steven Horwitz at Memorial Sloan Kettering in New York is excellent. So is Dr. Andrei Shustov at the Seattle Cancer Care Alliance in Seattle. There is a consortium of T-Cell Hematologists nationwide who pool their brain power against T-Cell malignancies. I would imagine (but am not certain) that one of their members is at MD Anderson.
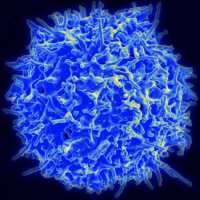
ALCL/ALK+ normally responds well to CHOP, even without the Etoposide added (CHOEP). I would then wonder about the pathology on your husband's biopsy sample. Lymphoma, for lack of a better term, can be diabolically hard to identify and mistakes are made. T-Cell Lymphomas are a very widely ranging set of malignancies that have little in common other than their origin in a T-Lymphocyte. Prognosis, treatment and outcomes vary significantly.
Thus, a T-Cell specialist (or constant consultation with one by your hematologist) is crucial to a good outcome.
0
Discussion Boards
- All Discussion Boards
- 6 CSN Information
- 6 Welcome to CSN
- 122.1K Cancer specific
- 2.8K Anal Cancer
- 448 Bladder Cancer
- 309 Bone Cancers
- 1.6K Brain Cancer
- 28.5K Breast Cancer
- 398 Childhood Cancers
- 27.9K Colorectal Cancer
- 4.6K Esophageal Cancer
- 1.2K Gynecological Cancers (other than ovarian and uterine)
- 13K Head and Neck Cancer
- 6.4K Kidney Cancer
- 673 Leukemia
- 795 Liver Cancer
- 4.1K Lung Cancer
- 5.1K Lymphoma (Hodgkin and Non-Hodgkin)
- 239 Multiple Myeloma
- 7.2K Ovarian Cancer
- 65 Pancreatic Cancer
- 490 Peritoneal Cancer
- 5.5K Prostate Cancer
- 1.2K Rare and Other Cancers
- 543 Sarcoma
- 738 Skin Cancer
- 658 Stomach Cancer
- 192 Testicular Cancer
- 1.5K Thyroid Cancer
- 5.9K Uterine/Endometrial Cancer
- 6.3K Lifestyle Discussion Boards