SWENZKE~Have chosen 2 answer your ltr here so other Peritoneal cancer patients can benefit by it as

(Note: Referencing "Swenzke" entry, http://csn.cancer.org/comment/1557289#comment-1557289, I would like to place my answer here so more people can gain help from this rare cancer known as Peritoneal Carcinoma. You may see her original letter there."
____________________________________________________________________________
Good afternoon “Swenzke”
First of all, thank you for giving me a background of your mom’s cancer journey thus far. You can read more “about me” by “clicking” on the picture of me and my husband, William in the blue square on your left. But for now, although it is difficult for me to be brief, I am also often times “blunt” and this will be one of those times. So in this very first paragraph, I will tell you that just like “time waits for no man”, neither does cancer, and all the more so for Stage IV. Time is of the essence for your mother, as it is for me in this present moment.
I have just had a PET/CT scan two weeks ago now, and my consultation with the oncologist to discuss the findings was last week. My original diagnosis was Peritoneal Carcinomatosis back in November of 2012. A second opinion at the University of Pittsburgh Medical Center also indicated cancer was in my Ovaries as well. Well, even before the discovery that the ovaries were infiltrated, the first diagnosis of Peritoneal Carcinomatosis put me in the Stage IV category. That meant that tumors were freely flowing around in the peritoneal fluid of my abdomen. UPMC did exploratory surgery and indicated that tumors were too numerous and too large to perform surgery right away. They recommended chemotherapy of Carboplatin and Taxol. This I did as soon as I returned home.
Just like your mom, the chemo worked well for me. It reduced my tumors enough for Cytoreductive Surgery. On July 1, 2013, I was admitted to University of Pittsburgh Passavant Hospital. There Dr. David Bartlett performed the surgery and removed all “non-essential organs” in my abdomen, which included my spleen, gallbladder, ovaries, fallopian tubes, omentum and sections of my intestines. Previously at age 36, I had my uterus removed. At age 12 I had my appendix removed. Those two organs would have been removed as well, if I had still had them at the time of my Cytoreductive Surgery (CRS) commonly called “debulking”. These were all organs within the abdominal cavity to which the cancer could potentially spread. It was a hard surgery, but thank God I survived.
In the Fall of 2014, scans revealed 3 tumors on the Caudate Lobe of my Liver. Cyberknife surgery (targeted radiation) in September of that year was a complete success.
In June of 2015, another scan revealed “increasing nodularity along the intestinal wall.” I was bordering on Intestinal blockage. So once more I underwent a series of chemo treatments consisting of Carboplatin and Paclitaxel (Taxol). That was completed September 25, 2015.
All along I have been seeing my oncologist on a regular basis. Since I have DVTs in both lower extremities, I am on Coumadin (Warfarin). I prefer that to other anti-coagulants on the market today. I am constantly monitored to see that my blood remains at the right consistency.
About 6 weeks ago now, I had a “rougher week” than normal. Actually, there are actual times when I almost forget that I have Stage IV cancer, except that I have problems with irregularity, which one can get used to, although very unpleasant. I am not as strong physically as I once was. But that’s to be expected. But one week I actually was sick enough to know that I am a terminal cancer patient. So I asked my doctor for a new scan, and he ordered a PET/CT scan. The results were tumors in lots of new places.
Compared to my last PET scan in June of 2015, my new PET scan dated Oct. 3, 2016 revealed that I now have:
- New malignant lymph nodes in right posterior lower neck
-
Posterior right paratracheal lymph node thoracic inlet (malignant)
-
New malignant adenopathy middle mediastinum
-
Small volume new malignant subcarinal adenopathy
-
Small bilateral pleural effusions and there is basal hypermetabolic activity in the pleural space on the right
-
Prior Pleural effusion increased
-
Diffuse serosal surface tumor abdomen and pelvis
-
Perigastric disease (potential for gastric wall invasion/involvement, including lesser sac region
-
Transverse mesocolon region
-
Deep pelvic deposits, other sites.
-
This is overall significantly worse compared to June of 2015 (more widespread) although a few sites have interval improved. Compared with CT scan in June of 2016, gastric wall or serosal disease has worsened, with thickness of antrum 5.6 cm presently versus 3.6 previously.
There are other findings but I just thought I would give you an idea of how cancer spreads. In December of 2015 my CA125 count was down to “8”. Last count was 340. I’ve never had a high count but my report shows you just how bad the cancer can be on the inside with a low count. So although some people seem to have a “high CA125” level, it is NOT the sole determining factor as to what’s actually going on inside.
Now so far I have no intestinal obstruction or gastrointestinal obstruction although I have been having heartburn lately, which is a new development for me. This report was just issued ten days ago (Oct. 4th).
My oncologist says chemotherapy should start ASAP. Hope that answers your question. It answered it for me.
As for me, we discussed clinical trials. He mentioned possibility of two different ones, but one did not have an opening until the first of the year, and he said that I didn’t have the luxury of waiting that long. The other trial that I could enter did not have a good success rating thus far. About 30% show some improvement. Along with the low possibility of improvement, he said applicants were very sick for the first two months of entering the trial, but after that the conditions improved. He did know of one person that had really great improvement and was still feeling well 4 years later. With that particular one, the patient would have frequent biopsies taken of one of the same cancerous nodes to determine improvement, or lack thereof, for the chemical that was being given. I ruled that out. I figured, “Okay I already have terminal cancer. If I enter this trial which is open, and I am one of the 70% with no improvement, then I have subjected myself to more pain and suffering for 2 additional months with the possibility of not having a good result. I felt the odds were too low. That was a gamble I was not willing to take.
So that left me with opting to go on a different chemo called Doxil, or go for a 3rd round of treatments of Carboplatin/Taxol. (Usually the Carbo combo is the traditional first treatment recommended for both Peritoneal Carcinomatosis and Ovarian cancer.) Now with each subsequent chemo regimen, effectiveness will decrease and toxicity increase. But since I’ve been a year without the chemo of Carbo/Taxol the oncologist felt that I might yet benefit by another series of that same treatment. My husband and I had come to that conclusion before he told us that this is what he was leaning toward. So we took that as a confirmation that this is what we will “go with yet again.”
Now I don’t mind telling you that I am not looking forward to this because there will be times when I will be extremely weak, with all the possibilities of side effects not previously felt. Now my hair has just grown to be about 5 inches long and I was beginning to look more like a female. Yet hair loss is a plus if the chemotherapy is working to reduce the level of infiltration of the cancer. And so this coming Thursday, October 20, 2016, I will be entering my 3rd round of chemo treatments. There will be 6 treatments, each 3 weeks apart. Chemo has a residual effect of 3 weeks, so tests are normally done 3 weeks from the end of the complete cycle. I am a realist and my hope is that this will afford me a longer period of “progression free survival. (PFS)” This is ALL that I, as a Stage IV patient can hope for. So all these drugs are designed to “tamp down” the spread of the cancer and hopefully keep it from coming right back again. I am happy to have had a year’s reprieve before having another treatment.
Now chemo is not a magic bullet, and at some time, depending on the intensity of infiltration of the cancer for each patient, it will NO longer be effective. So it is up to the patient to decide when enough is enough. Currently there are clinical trials ongoing for this cancer, but NONE have been APPROVED by the FDA for use among the general population. I receive lots of medical alerts on a daily basis dealing with oncology. I copied out one called “NiraParib”. I spoke to my oncologist and that is not yet available for a clinical trial here, but he was familiar with it.
There are different clinical trials going on now here at Virginia Oncology, but none that I would be qualified for. So it may be that after my Carbo combo treatment, something would become available, or that I might elect to enter a clinical trial. But the bottom line should always be “quality of life” rather than “quantity of life.” I don’t intend to “kill myself” with continual debilitating treatments that lessen my quality of life till life isn’t worth living. That’s how I feel. I am a Christian, and know where I’m going when I leave this earth. I make no apologies for giving credit to the Lord for my survival thus far. So far the treatments and the pain have been “worth living for.” My family and friends are all important to me. Everyone knows that this is a terminal situation, and they, my doctors and I, are happy to see me feeling this well so far out from my original diagnosis. After all, I could have died within 6 months, so I consider myself “blessed” although I’m not certainly worthy of any special grace. I have never moaned and complained and said, “Why me? This isn’t fair! Life’s a b_i_t_c_h! That’s just a few of the words I have heard uttered from cancer patients. Well, I say, “Why not me?” I’ve been given a peace of mind and heart that is unexplainable and it is due to my absolute faith in the Lord. He has promised to never leave me or forsake me, and that is the basis for my positive attitude even though all things on the inside of my physical body are “negative.” I have “soul peace”. Without that, no doubt, I would be a “basket case” with no hope of here or the hereafter.
Like your mother, I, too, had a severe reaction to the Carbo/Taxol treatment the very first time. I actually thought, “I think I’m dying.” I told that to the nurse, and she said, “I won’t lie to you. We have coded some!” I was there from 8:15 A.M. till around 7:00 P.M. that night. The oncologist stayed with me the entire time. They snatched off the lines and immediately began treatments to counteract the severe reaction I was having. My husband said my body turned completely “red” all over. I was in the restroom at the time. I had just been “hooked up” and thought, “I think I should go to the restroom.” It had not been 2 minutes until I began to feel faint and dizzy. I told my husband, I’m going to pass out. My legs were giving away. The nurse was right outside the door. She immediately put me in a chair and several rushed to my aid. THIS WAS SCARY! But I lived to “endure” another day. I am left with some permanent neuropathy from the very first treatment, but like I say, it knocked back the tumor growth.
So now I’ve shared my experience with you. I STRONGLY recommend that your mother start the treatments IMMEDIATELY. My oncologist told me yesterday, it is wise to start ASAP. He said I would not wait till the first of the year. I had also asked about waiting until I could go visit some of my relatives that live on the other side of Virginia.
Lastly, I think that both your mother and I will have the prospects of a much Merrier Christmas and a Happier New Year if we “bite the bullet” and “get on with trying to kill the cancers NOW.”
You ask, “Are things worse than they could be, am I in denial? My mom lives with my husband and I and our 4 kids - we have an in-law suite. Do I let her travel and go visit her other daughters (1 lives in Canada, the other in Boston) or do we need to start the chemo ASAP?” Number One I think that you are not as much in denial as you are just unaware of the severity of how fast this cancer can travel. I would say that if you were in “denial” you would be arranging travel plans instead of wondering about which was more important, chemo or visiting family and friends.
Acceptance of our cancer is the first step toward getting the best treatment. It is good that you have an in-law suite. Secondly, if your mother will listen to “reason”, she should NOT go to visit her other daughters. Travel should be delayed. May I ask, “Can the daughters come to see their mom at your house?” Maybe even more convenient for you, they could get a hotel room close by, could they not? You will have all the work you need tending to your mom’s needs. Bottom line, YES, you need to start the chemo ASAP. (I say, IF your mom will listen to reason for this reason. Myself included, I find it harder to allow someone else to tell “me” what I should do. I am now 77 and well on my way to being 78! And I found that to be true with my own dear mother, the older she got, the more adamant she was about being “independent” when in fact she was becoming more dependent on the family members than ever before. She went to be with the Lord at age 99. I miss her still. So “kudos” to you if your mother is taking your advice in the way she should. Look I know you love your mother, or you wouldn’t be writing here, but it takes a lot out of the caregiver’s life to set aside your own plans to take care of your mom.
I have been both a caregiver to my husband when he was diagnosed with Esophageal Cancer back in 2002. Thank God he is a survivor. Otherwise, who would be my caregiver? We’ve now changed rolls, and he is my caregiver, and a wonderful one. I am not going to live forever and our love has only grown stronger. Cancer will either tear families apart or bring them closer together. It also enlarges our capacity to care for others who are even in worse shape than I am presently in. After all, I could be blind, crippled, mentally incompetent, homeless, without good medical treatment or even live in a foreign country. There’s no better place to live than in the USA. God has indeed blessed our country, although many have forgotten how blessed we are. And one more thing, I don’t live in North Carolina, I live in Virginia and have had considerable flood damage to parts of my home but at least the water isn’t up to the rooftop, so we can always take a look around, and just be content to cope with our own problems. That’s my attitude. So we always count our blessings along with the things we have to contend with at the time.
Since I relate completely with your mom’s diagnosis, and are seemingly in a similar place as far as needing treatments is concerned, I trust you will consider what I have said to be sincere, compassionate, straightforward and yet informative. I will give you some references below my name which I think should help. I wrote a letter to a fellow named Brian previously about things that helped me during my previous chemo treatments, so I will include that link as well as the one for one of the newer clinical trials which has now completed 3 necessary phases, and is waiting on receiving FDA approval.
It truly is my prayer that your mother will be able to undergo this series of treatments with the least complications and yet with great results.
Loretta Marshall
Peritoneal Carcinomatosis/Ovarian Cancer Stage IV
_______________________________________________________________
Things to know about the Peritoneal Cavity
_________________________________________________________________
2. 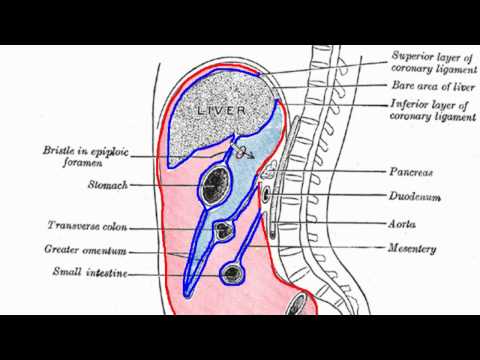 https://www.youtube.com/watch?v=Uo3jDAXR_Ww
https://www.youtube.com/watch?v=Uo3jDAXR_Ww
Video – tutorial on the Peritoneum
_______________________________________________________________
3. http://www.nejm.org/doi/full/10.1056/NEJMoa1611310#t=articleTop
Successful Phase 3 of clinical trial for “Niraparib” for Ovarian cancer, Stages III and IV
_______________________________________________________________
4. http://www.oncolink.org/blogs/2016/08/protein-requirements-cancer-patients/
This is an informative 10-minute video on the importance of protein in a cancer patient’s diet
__________________________________________________________________
5. http://csn.cancer.org/node/301646
My answer to Brian from the North’s letter inquiring about tips for his mom’s first chemo treatment.
_______________________________________________________________
6. http://www.cancer.net/cancer-types/ovarian-fallopian-tube-and-peritoneal-cancer
Overall topics relative to these cancers
__________________________________________________________________
7. http://www.cancer.net/cancer-types/ovarian-fallopian-tube-and-peritoneal-cancer/stages-and-grades
Specific stages of Peritoneal Cancer
_____________________________________________________________________
8. http://www.cancer.net/cancer-types/ovarian-fallopian-tube-and-peritoneal-cancer/treatment-options
Treatment options relative to stage
_____________________________________________________________________
9. http://csn.cancer.org/node/302908
My letter written on the Ovarian Cancer site: Are we not all Gamblers playing in the Cancer Casino hoping 2 win Life's Lottery~but what if? In this letter I include a very in-depth article written by the Mayo Clinic about when to consider stopping treatment and the different reasons for “when or why”.
_______________________End of references____________________
Comments
-
Updates!
OK, after some strong coaxing on my part, my mom said up an appointment with another doctor she had used previously. She starts chemo again on Nov. 14, 2016. The doctor is hoping to be able to use Avastin this time because of her difficulty with Taxol. I am not sure if they will be increasing the dosage so chemo will only be once every 21 days or if it will be 3 weeks chemo, 1 week recovery again. She has another cat scan scheduled for today and we will be seeing the doctor again on Monday Nov. 7 to discuss her options. The doctor informed us that he may not be able to get Avastin approved.
0 -
Swenzke~U did a good thing~Mama didn't raise no fool as they say
Hello again Swenzke,
Thanks for coaxing your mom and pushing her in the direction she NEEDED to go. Vacations must take second priority to medical necessities!
This is a wise decision. Let us know the results of the scan. Frankly, I like going once every 3 weeks for chemo. My regimen is for 6 treatments, each one 3 weeks apart. And remember to ask for hydration afterwards. I get the Neulasta injection which keeps my white blood count from dropping to a point so low that I have to miss a treatment. As for Avistan, it doesn't work well for lots of people, and has tremendous side effects which to me, hold more possibilities of additional problems that I'd rather not deal with. Often the effects are seemingly worse than the condition one is trying to improve! And a word of note here, people look at me and say, "You sure don't look sick." Well, I am, and that's why we NEED scans so doctors can see on the INSIDE although we look okay on the OUTSIDE. That certainly gives true meaning to "looks can be deceiving!"
Loretta
0
Discussion Boards
- All Discussion Boards
- 6 CSN Information
- 6 Welcome to CSN
- 122.1K Cancer specific
- 2.8K Anal Cancer
- 448 Bladder Cancer
- 309 Bone Cancers
- 1.6K Brain Cancer
- 28.5K Breast Cancer
- 398 Childhood Cancers
- 27.9K Colorectal Cancer
- 4.6K Esophageal Cancer
- 1.2K Gynecological Cancers (other than ovarian and uterine)
- 13K Head and Neck Cancer
- 6.4K Kidney Cancer
- 673 Leukemia
- 795 Liver Cancer
- 4.1K Lung Cancer
- 5.1K Lymphoma (Hodgkin and Non-Hodgkin)
- 239 Multiple Myeloma
- 7.2K Ovarian Cancer
- 65 Pancreatic Cancer
- 490 Peritoneal Cancer
- 5.5K Prostate Cancer
- 1.2K Rare and Other Cancers
- 543 Sarcoma
- 738 Skin Cancer
- 658 Stomach Cancer
- 192 Testicular Cancer
- 1.5K Thyroid Cancer
- 5.9K Uterine/Endometrial Cancer
- 6.3K Lifestyle Discussion Boards