Esophagectomy - what now?
Comments
-
Thank you, CorgiMom. I'llCorgiMom said:high calorie product
I started working with a nutrionist last week to fine tune my diet so I get more nutrient/calorie dense foods. While I don't dump Ensure, it does make my pulse race and saps my energy. I think it's the sugar spike. My nutritionist suggested a product called Benecalorie and I've ordered it. It comes in powder & liquid and a single 1.5 oz serving packs 330 calories. Reviews say it's mostly tasteless. I'm anxious for the order to arrive & try mixing it with soup or a shake. Maybe you can investigate & if I can remember after trying it, I'll report back.
Thank you, CorgiMom. I'll have a look at this product.
0 -
I was going to recommend Benecalorie as wellcsacerdote said:Thank you, CorgiMom. I'll
Thank you, CorgiMom. I'll have a look at this product.
Benecalorie is basically tasteless and calorie dense. You can typically find it at Walmart
Benecalorie is made by Nestles and they have an web site dedicated to cancer diet support.
Best Regards,
Paul Adams
McCormick, South Carolina
DX 10/2009 T2N1M0 Stage IIB - Ivor Lewis Surgery 12/3/2009
Post Surgery Chemotherapy 2/2009 – 6/2009 Cisplatin, Epirubicin, 5 FU
Six Year Survivor0 -
Question regarding Digestion
With reference to Benecalorie, I've since learned olive oil (and other oils) is about 120 calories per tablespoon. So I've been mixing 3 tablespoons with yogurt which brings a serving up to almost 500 calories. It doesn't change the taste or consistency considerably either.
I don't wish to "gross anybody out" here. But there is another question I need to ask...
Since beginning to eat solid foods again, my stools have been soft and yellow in color. I've read that this could be an absorption problem, and might explain why I'm often fatigued. Have any of you had the same experience, and did it improve over time?
Thanks,
Craig
0 -
Digestioncsacerdote said:Question regarding Digestion
With reference to Benecalorie, I've since learned olive oil (and other oils) is about 120 calories per tablespoon. So I've been mixing 3 tablespoons with yogurt which brings a serving up to almost 500 calories. It doesn't change the taste or consistency considerably either.
I don't wish to "gross anybody out" here. But there is another question I need to ask...
Since beginning to eat solid foods again, my stools have been soft and yellow in color. I've read that this could be an absorption problem, and might explain why I'm often fatigued. Have any of you had the same experience, and did it improve over time?
Thanks,
Craig
Hello Craig,
I've had diarrhea for coming in on 5 years now. I actually went 3 1/2 years with a minimum of 3 trips per day (that's EVERY DAY for 3+ years). I have taken 5 different meds for it and have struggled with that vs. reflux. One med I take is to flush things through my system and another is to keep it in. Coming in on 5 years, I think I may have actually struck a workable balance. It can certainly cause fatigue as you aren't receiving the nutritional benefit you expect from the food you are consuming. Maximizing calories actually used is an important thing. Only you will know that, for example, olive oil gives you more of a caloric benefit vs. a diarrhea loss. You may want to work with a certified nutritionist at the hospital you got to to find what's best for you. People's isolated, anecdotal experiences are less likely to be useful to you as a professional working with your own experience.
Best of luck with it,
Ed
0 -
It could be several things??
Craig,
Different colored stools could be a number of things. Light stools could just be a function of your diet in general, if you are eating a lot or dairy items or soups and broth etc., it could have that effect. If your stools are pale or clay-colored, you may have a problem with the drainage of your biliary system, which is comprised of your gallbladder, liver, and pancreas. Bile salts are released into your stools by your liver, giving the stools a brown color. A yellow looking stool may be the result of fats not being completely absorbed by your new digestive system. There is unfortunately a section of the “LiveWell” web site dedicated to the various colors your stool may exhibit https://www.unitypoint.org/livewell/article.aspx?id=d7a92af5-f39d-46fa-81ef-a17dce49788f
The best approach would be a discussion with your PCP or Oncologist because there are also some medications that can change the color of your stool.
Best Regards,
Paul Adams
McCormick, South Carolina
DX 10/2009 T2N1M0 Stage IIB - Ivor Lewis Surgery 12/3/2009
Post Surgery Chemotherapy 2/2009 – 6/2009 Cisplatin, Epirubicin, 5 FU
Six Year Survivor0 -
Craig~Glad U R eating~? U ask may just B normal for post-op EC!
Hello Craig ~
Hey glad to hear you’re FINALLY getting something solid to eat. It will take a while for your body to “settle in on its new pattern of “normal.” Regarding your specific question relative to stool color and consistency you describe, they are not uncommon with people that have had gastric surgery. I’ve not discussed this specifically before, but this is common when parts of our body have been removed that were originally placed there by our Creator!
In my own surgery for Peritoneal Carcinomatosis the surgeons said they would remove all “non-essential organs.” Now I had already had my appendix removed at age 12 and removal of my uterus at age 36. I suffered no ill effects from those surgeries. But when I had my ovaries, fallopian tubes, omentum, spleen, gallbladder and portions of my intestines removed, it has definitely changed the way my body processes food and also effects the consistency, color and frequency of bowel functions. And in the same way when one has had an Esophagectomy, it is gastric surgery, and in my husband’s case, affected both the color, consistency and way elimination processes took place for him as well.
Each time my husband has a CBC it shows that he is slightly anemic. His gastroenterologist says that it is just the way my husband’s body processes food. I don’t remember the exact term he used, but it did have to do with the way the body absorbs and processes the nutrients that are consumed. The Gastroenterologist did not suggest any kind of medication in the case of my husband.
Incidentally, my husband goes down to the Red Cross and gives blood platelets twice monthly and has always tested “okay” for donations.
So I have looked at several sites that pretty much explain the same things that Paul talks about. In my husband’s case, the gastroenterologist was not upset about the “anemic” finding and suggested that it was a natural side effect in some patients that had had an Esophagectomy. Now we’re talking 14 yrs. ago, and things haven’t changed. Since there are only “adults” in the room, let me say that one can eat nutritious foods and yet the color of the stools can still be “soft and/or tan colored or yellow”. You can “run that by” your surgeon or GP, but I believe he may well tell you the same thing.
But remember Craig, we don’t want to “lose our license to comment, compare or suggest”, lest some complain that we are “diagnosing and treating” conditions that we’ve not been licensed to treat. (Paul you can “read between the lines here” :). We always like to say, this is what we know “experientially.” We are not doctors and always suggest you ask your doctors about anything that we may say from our own experiential and personal point of view. You can compare your symptoms with other patients and probably conclude that you’re “normal”. Regularity should prevail with the passing of time, and yet the stool color and/or consistency may still remain the same and will not necessarily “change” with time.
But for the record, I will put some links below my name that will explain how patients that have had cancer and/or gastric surgery can experience changes in the color of bowel movements and frequency! (The Cleveland Clinic and UPMC) are similar in describing why “dumping” occurs. This was one of the first problems we encountered when my husband began to eat solid food soon after his MIE surgery.
And it doesn’t always have to be that “something is wrong” with you, it may just be that the “parts of your body” are not going to function in exactly the same way as they once did, because they are “missing” in action! Some bodily functions simply change after an Esophagectomy. But you learn that they are “trade-offs” for surviving. You learn to adjust and live with the changes.
Hope this helps.
Loretta (William's wife) William EC Stage III (T3N1M0) adjuvant chemo/radiation then Ivor Lewis Minimally Invasive Esophagectomy (MIE) by Dr. James D. Luketich on May 17, 2003. William now into 14th yr. of survival cancer free!
_____________________________________________________
This is a Dietary Guide for post-op EC patients
"Diet After an Esophagectomy
An esophagectomy (ee-soff-uh-JEK-tuh-mee) is surgery to remove the esophagus. After this type of surgery, it is common to have some problems eating for a few months.
What can I expect after surgery?
For the first few months after surgery, you may have problems such as:
Weight loss - Dumping syndrome (nausea, diarrhea, abdominal cramping, light-headedness) - Excess gas - Trouble swallowing
-
Your diet plan after surgery is designed to lessen your discomfort and allow you to enjoy eating…”
____________________________________________________
Tips to deal with dumping syndrome which occurs in lots of Esophageal Cancer patients post surgery
2. http://www.upmc.com/patients-visitors/education/nutrition/pages/dumping-syndrome-diet.aspx
“Dumping Syndrome Diet
Dumping syndrome sometimes happens after stomach surgery.
Dumping syndrome is caused by large amounts of food passing quickly into the small intestine. This causes symptoms like abdominal pain, cramping, nausea, diarrhea, dizziness, weakness, rapid heartbeat, and fatigue. This diet will help stop the symptoms of dumping syndrome.
Tips to Help Relieve Symptoms…”
__________________________________________________________
Now we know that you’ve been in a great deal of stress, who wouldn't be? However, I think that most of your bowel problems are mainly as a result of your Esophagectomy and new adaptation to eating
3. http://www.healthline.com/health/digestive-health/yellow-stool#Causes3
“…Stress
Part of your body’s response to stress and anxiety may be to speed up the digestive process. This limits the volume of nutrients your body can absorb, and may cause diarrhea and yellow stool…
Part 2 of 5: Color - What gives stool its color?
Bilirubin and bile give poop its normal brown color. Bilirubin is a byproduct of your red blood cells. It’s produced in the liver and then moves to the gallbladder, where it mixes with bile. From there, most of the bilirubin passes into your intestines where it’s broken down by bacteria and discarded in your feces or urine…”
_________________________________________________________
I’ve included this just in case your complete blood count (CBC) indicates you’re a wee bit anemic. It could result from an “absorption problem”.
4. https://medlineplus.gov/ency/article/000584.htm
Iron deficiency anemia - “Anemia is a condition in which the body does not have enough healthy red blood cells. Red blood cells provide oxygen to body tissues. There are many types of anemia.
Iron deficiency anemia occurs when your body does not have enough iron. Iron helps make red blood cells…”
_________________________________________
5. http://my.clevelandclinic.org/health/diseases_conditions/post-gastrectomy-syndrome-overview
"Post-Gastrectomy Syndrome
The primary function of the stomach is to act as a reservoir, initiate the digestive process, and release its contents gradually into the duodenum so that digestion in the small bowel is optimally performed.
Causes
Patients with a diagnosis of gastric cancer, trauma, or complicated peptic ulcer disease may require a gastrectomy, which is the surgical removal of a portion of or, on occasion, all of the stomach. The anatomical changes that result after gastrectomy affect the emptying time of the stomach. If the pyloric valve located between the stomach and first part of the small intestine (duodenum) is removed, the stomach is unable to retain food long enough for partial digestion to occur. Food then travels too rapidly into the small intestine producing a condition known as the post-gastrectomy syndrome.
Symptoms
This syndrome is characterized by a lowered tolerance for large meals, rapid emptying of food into the small intestine or “dumping,” abdominal cramping pain, diarrhea, lightheadedness after eating as well as increased heart rate and sharp drops in blood sugar levels.
In the "early" dumping syndrome, symptoms occur approximately one-half hour after eating whereas in the “late” dumping syndrome they appear two to four hours after eating.
The carbohydrate component draws water into the intestinal lumen causing sudden fluid shifts in the early dumping whereas late dumping is caused by a reactive hypoglycemia. An estimated 25-50% of all patients who have undergone gastric surgery have some symptoms of gastric dumping. The incidence and severity of symptoms are related directly to the extent of gastric surgery.
Complications
Complications of post-gastrectomy syndrome include anemia as a result of vitamin B12 or iron malabsorption and osteoporosis.
These problems generally occur months or even years after gastric surgery. Vitamin B12 malabsorption occurs when a protein known as intrinsic factor is either not produced by the stomach (this is a condition called pernicious anemia) or when the proximal stomach is resected (the portion of the stomach that produces intrinsic factor). In either case, that absence of intrinsic factor leads to the poor absorption of vitamin B12.
Under normal circumstances intrinsic factor binds to vitamin B12 and assists with the absorption of this vitamin in the lower portion of the small bowel. When vitamin B12 is poorly absorbed, anemia and, in some cases, poor nerve function can occur. This generally does not happen for several years because vitamin B12 is stored in large amounts in the liver.
Iron deficiency anemia develops because removal of the stomach often leads to a marked decrease in the production of gastric acid. This acid is necessary to convert dietary iron to a form that is more readily absorbed in the duodenum. Anemia usually does not occur for a few years after gastric surgery because iron is stored in moderately large amounts in the bone marrow, where red blood cells are produced.
Osteoporosis develops as a result of poor calcium absorption, another problem that occurs after gastric surgery. Under normal circumstances, calcium absorption, which occurs in the duodenum and proximal small bowel, is modest at best, with large amounts being lost in the bowel movement.
Following gastric surgery, calcium absorption is even less efficient as a result of rapid emptying of the stomach. Calcium also binds tightly to unabsorbed dietary fat which further interferes with its absorption. Symptoms of osteoporosis may develop ten or more years after gastric surgery because of the large amount of calcium that is normally stored in bone.
Treatment
Treatment of post-gastrectomy syndrome includes initiation of a post-gastrectomy diet, which is high in protein, low in carbohydrates, and low in concentrated sweets. This diet should be consumed as five or six small meals, with limited fluid intake during meals. On occasion, medications may be required to help control these symptoms. Vitamin B12 deficiency can be prevented by providing vitamin B12 shots once each month indefinitely. Oral iron and calcium supplements are often needed to prevent the development of deficiencies in these minerals.
_________________________________________________________________
6. http://www.healthhype.com/stomach-dumping-syndrome-causes-symptoms-treatment.html
What is dumping syndrome?
Dumping syndrome is a condition where food from the stomach is pushed out of the stomach too quickly. It is also known as rapid gastric emptying. The exit of food from the stomach is carefully controlled by a number of factors outlined in normal stomach emptying. This process plays an important part in overall digestion. If it is too fast (rapid gastric emptying) or too slow (delayed gastric emptying) the digestion is affected in several ways.
Since foods enters the small intestine too quickly and without being adequately digested, most of the symptoms of dumping syndrome are noticed shortly after eating and can last for several hours. Dumping syndrome is mainly seen in people who had surgery to remove either part of or the entire stomach, or in gastric bypass surgery for weight loss. It can be managed with dietary changes although medication and surgery may be needed for severe cases.
Causes of Dumping Syndrome
The stomach is a large muscular sac that can distend to comfortably accommodate about 1.5 to 2 liters (around 50 to 70 ounces) of food and fluid. The stomach outlet is a narrow tapered portion known as the pylorus and connects to the duodenum of the small intestine. It is the pylorus that regulates the outflow of food and fluid from the stomach. In this way food and fluid can be adequately digested and absorbed at a steady rate.
Essentially the stomach acts as reservoir for food and fluid, slowly releasing it into the small intestine over time. However, with surgery this is affected in several ways. The surgery may affect the body of the stomach known as the fundus thereby reducing its capacity or there may be impairment of the pylorus thereby affecting the regulated outflow of stomach contents. The sudden influx of food into the small intestine can lead to host of adverse effects.
The reasons for stomach surgery may vary like for weight loss (bariatric surgery) or cancer. The procedures where dumping syndrome may later occur includes:
Gastrectomy - Gastroenterostomy or gastrojejunostomy - Gastric bypass surgery (Roux-en-Y operation) - Esophagectomy - Fundoplication - Vagotomy
Gastric dumping syndrome is more likely to become apparent once a patient who underwent surgery returns to a normal diet. Certain foods are more likely to trigger symptoms, particularly refined foods. Gastric dumping syndrome is also more likely to occur in people with certain conditions like diabetes mellitus and Zollinger-Ellison syndrome. Drugs like metoclopramide are used to speed up gastric emptying but normal emptying returns once the drug is discontinued.
Signs and Symptoms
The symptoms of dumping syndrome can be separated into early and late form. In the early form, symptoms usually appear within 10 to 30 minutes after eating although some symptoms may become apparent almost an hour after the meal.
In the late form, symptoms appear between 1 to 3 hours after eating. While both forms can affect a person, some people may only have one form like late dumping syndrome and not the other.
Early Dumping Syndrome
The body’s response to the sudden inflow of food into the small intestine gives rise to digestive and cardiovascular symptoms. The latter occurs due to hormonal responses as well as the sudden flow of blood to the intestines. These symptoms may include:
Nausea - Bloating - Abdominal pain - Intestinal cramps - Loud stomach noises - Diarrhea (arises after the other symptoms) - Flushing (face) - Rapid heart rate – Palpitations - Dizziness and sometimes fainting
Late Dumping Syndrome
The symptoms of late dumping syndrome arise from the body’s hormonal response to the sudden entry of large amounts of food in the small intestine and rapid absorption of nutrients. A surge in insulin causes reactive hypoglycemia. These symptoms include:
Hunger – Palpitations – Sweating – Tremors – Fatigue – Confusion – Agitation - Fainting
Complications
Severe dumping syndrome can lead to a host of complications.
Severe weight loss as the body cannot absorb sufficient nutrition.
- Malnutrition due to the impairment in digestion and absorption.
- Chronic diarrhea which has physiological and social effects.
- Persistent fatigue due to insufficient nutrients.
Diet for Dumping Syndrome
A few simple dietary changes can be useful in managing dumping syndrome without any medical intervention. These dietary habits need to be continued lifelong.
Eat smaller meals more frequently. Rather opt for 5 to 6 small meals during the course of the day rather 3 large meals.
- Chew thoroughly. By chewing thoroughly the food is broken down into smaller pieces and this helps with digestion.
- Limit carbohydrates. Refined sugar in particular is a problem but even natural sugars like lactose should be limited.
- Increase dietary fiber. Fiber helps to slow down the absorption of carbohydrates. High fiber foods should be included in the diet but if necessary, fiber supplements may be used.
- Lie flat after eating. Although this is not usually advisable, with dumping syndrome it can help slow down digestion by counteracting the pull of gravity.
____________________________End of references______________
0 -
-
Thank You
Thank you all for your time and input - I certainly appreciate it.
0 -
Getting Back to "Normal" some practical hints
Hi, Rhonda. I had an esophagectomy almost 5 years ago, and I am *still* adjusting (in a good way). Over our lives, I think we all make diet and excerise adjustments, simply as part of living. Well, this continues, so it is not a "bad" thing. It's just another phase of adjustments. I didn't get much advice at the beginning, reading very much the same advice you (from here on, when I say "you", I mean your Dad.) have now received, but I never really understood what it meant. So initially, I tried to eat the same type of food that I always did, adjusting to quantity (I thought) and ease of digestion. I had a lot of trouble. Over time, however, I learned, much as Pavlov's dogs did, that it wasn't worth it. These are significant: Dumping syndrome, acid reflux (directly into the mouth now, often breathed into the lungs, a horrible experience), vitamin B12 deficiency (feeling light-headed), hypoglycemia (also includes feeling light-headed, but more shaky). Carobonated drinks will "pressurize" the smaller stomach and cause discomfort, but can also produce this effect much later than you think, and contribute to the reflux pressure. So have the last one no later than 6 pm. The worst food group is fats. Not the so-called gas-producing veggies. Fats take a long time to digest and produce a lot of gas, especially later on in the digestive process. Dense proteins are similar but not as bad on acid. Steer clear as much as poss, but a little fat on a steak if eaten early enough, is OK. Dumping and hypoglycemia: because the pathway to the stomach is instantaneous, sugar gets digested immediately and can raise blood sugar very quickly. Insulin kicks in and plummets your blood sugar. I keep my sugar intake to about 15 gm max per session. (Lose the soft drinks. They can have 45 gm of sugar in them. VERY bad.) Periodically, I feel the effects of hypoglycemia. A little sugar fixes this, but leaves me quite tired for a while after. Once in a while, food just gets to the bottom of the stomach faster and presses the pyloric valve. This could trigger the need for a an evacuation (polite term), usually of the liquid type. Nothing to worry about unless you're in a restaurant or the boss's house. Hard to hold. Sorry, that's the icky part. Now, I eat "normally". That is, the new normal. Food stays in the digestive system for 24 hours or so, so I have learned to eat very lightly at breakfast and lunch, if at all. Don't forget that coffee, or even water, as you have discovered, is a substance, too. That is, it puts weight on the stomach and can make you feel quite uncomfortable. Clears up after 30 minutes or so, though. BUT it can add pressure to whatever has already been eaten, so postpone your coffeee or tea. Water is good. Try not to drink less than you should. I find I can eat one fist-sized mass of food comfortably. I can eat MORE, especially at dinner, which is a social ritual-type occasion, and hard to avoid. If I do eat more, however, I pay a price for about 2 hours after. Just discomfort, nothing serious. Like you have eaten a MASSIVE Thanksgiving turkey dinner all by yourself. Goes away, though. So, in summary: you will adjust over time, find foods you can eat, even if you shouldn't, in the quantities you want (the "want" part will gradually diminish, so no loss, really). Spicy foods aren't good, keep quantities low. My routine, quite successful, is a coffee first thing (who doesn't want that?), something small like a bagel, with butter or cream cheese. Then around lunch time I have a decaff coffee usually, try not to have any more food (it is AMAZing how little food we really need to function well - the food industry has blinded us). Sometimes I have the equivalent mass of another bagel, sometimes not. I actually sometimes just have the coffee, get some CHipwagon fries (small) around 11:30, then nothing till supper. Then, a "normal" size supper. I usually have a glass of wine around 10pm, sometimes with some toast (popcorn is a good snack food too).
I start out sleeping in a recliner, then find I wake up between 3 and 5, and move to bed, which is at about a 4 inch raise at the head. The relining, for me, has been ESSENTIAL. It is very hard to sleep in a hotel, even with pillows (I seem to naturally want to sleep on my stomach) without a reflux event. The only way I can help this is not to eat after about 4 pm. That's anything.
I, too, was amazed at what the surgeon had done. Take out an esophagus, pull up the stomach, and sew it in place. A - MAZEing. Endoscopically, in my case.
Today I function pretty much normally. The best thing to consider is attitude. Don't dwell on how hard it is and how special you are. It is what it is. Turn your attention to living, not wallowing. I had my funeral all planned, music, etc, thinking I wasn't sad or maudlin, just something to do. Well, I've got other things to do now, a little more constructive. Stop yourself feeling different IF you want to feel the same. That last sentence is the key.
Have fun
John
0 -
Eating and wierd throat sensations.
I am 57 years old. I was diagnosed with esophageal cancer in January of 2016, went through six weeks of chemo and radiation and had an esophagectomy in May. I was discharged from the hospital after 8 days with a feeding tube and the usual instructions. Soft foods, small meals, etc. My other instructions were to 'walk as much as possible' and 'get as much rest as possible'. Hard to do both, but I started walking short distances and have been walking about 2 miles a day for the past 2 months.
On to the Subject line. If I eat something really cold, I get what I can only describe as a 'clucking' in my throat when I swallow. It happens at other times, and it seems like I will lose my ability to swallow.
The other sensation is the feeling you get when you are first getting a sore throat. This 'tick' in my throat is almost always there. I have seen an ENT, he said nothing is wrong, just a part of healing. I still wonder.
My other issues are the same as the ones stated above. I was always active, worked hard physically, and now the simple things tire me out. The mind wants to do it, but the body says no.
Thanks to all for writing. I joined today and have learned alot already.
0 -
slj2859~Your problem may be as simple as a "dilation"-hope so.
Hello there –
Those of us who write here regularly have been dealing with some patients who do not have the good news that you have. So we’re glad to hear that you have been able to have a successful Esophagectomy and it would appear that you are adjusting well. I don’t know where you had your Esophagectomy, or what type you had, but I’m glad you’ve learned a lot by reading here. So far so good, wouldn’t you say?
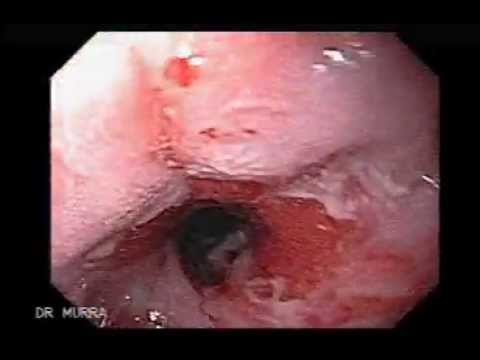
As for the “tick” in your throat, has your surgeon mentioned anything about a “dilatation” or “dilation”?
About two weeks after my husband’s Minimally Invasive Esophagectomy at UPMC, he began to clear his throat a lot. He would have a slight cough and clear his throat. Incidentally, my husband had very frequent follow-up visits after his surgery. I hope you have regular access to your surgeon and his medical team, as you need to have peace of mind as you adjust to your new normal.
So as soon as my husband mentioned how he was constantly clearing his throat but never able to “cough up anything” or “swallow” to get relief, Dr. Luketich had a logical explanation. He explained that it was not uncommon to have a slight scar tissue buildup around the area of the anastomosis (the junction at which the two organs are rejoined.) Dr. Luketich explained that it was like a “cup and saucer”. The “new elongated gastric tube” being the cup of course, and the “saucer” being a tiny ridge of scar tissue (a rim) on the inside of the tube. Saliva is always present inside our mouths. This little ridge was just enough to keep saliva or a speck of food from traveling all the way down the tube unhindered. In my husband’s case, it was only saliva. It was never a feeling of food getting stuck.
My husband, whom we call Bill at home, had his entire Esophagus removed, and the stomach was rejoined at the area of the pharynx (throat). This could be a logical explanation as to what you might be experiencing.
So Bill went in for a dilation. It was a simple outpatient procedure, in which the doctor inserted a device and gently stretched that area. (See the video below). It was nothing painful. The most one might experience is a “sore throat”. But that should disappear in a matter of 12 hours or so. In another month or so, he experienced the same slight cough and throat clearing problem. So Dr. Luketich performed another dilation. This occurred in the first two months following his Esophagectomy, and none has been needed since. So I hope that this is a simple solution to a common occurrence. The only thing being is that “you’ve never been down this road before, and you must always confer with your surgeon” when you have any questions, or symptoms that are unexplainable.
Here’s hoping this is a simple problem that can be cleared up with a dilation.
Loretta
Wife of William (Ivor Lewis Minimally Invasive Esophagectomy at University of Pittsburgh Medical Center on May 17, 2003 by Dr. James D. Luketich. We are blessed to be into year 14 of recovery from Stage III (T3N1M0), with no residual cancer to date.
______________________________________________________
Here is a video and an explanation of a balloon dilation. Yes it looks gross, but it’s a simple procedure.
1.
 https://www.youtube.com/watch?v=UPlMtKpld780
https://www.youtube.com/watch?v=UPlMtKpld780 -
Hi Jim (slj2859):
Hi Jim (slj2859):
My story is similar to yours - even the timeline - although I had some serious complications following surgery. I found the recovery and adjustment period is far longer and more difficult than the doctors lead you to believe.
It's only in the last 6 weeks that I finally figured out a diet that works for me and started putting on weight again. The doctors send you their canned dietary recommendations. But within these recommendations, you really need to figure out the foods that work for you. e.g. They recommend Ensure+, which unfortunately goes right through me!
I get similar sensations in my throat, and need to be mindful of what I'm eating/drinking, its temperature, how much, and how quickly. e.g. Eating a large portion of very hot or cold food too quickly can cause considerable discomfort. In my case, I've also found that I need to let myself burp after several swallows. That seems to "clear the path" into my stomach. This is all the "new normal" for me, which I don't particularly enjoy. But I'm getting used to it, and guess at some point I won't even think about it anymore.
Regarding your energy level, my experience has been the same. However, it should improve after your diet stabilizes. At this point I haven't nearly the energy I had a year or two ago. But I have far more than a month or two ago. It WILL get better.
Good luck to you, Jim.
Craig
0 -
EC and Ivor Lewis Procedure
http://thetanseys.webs.com/Cancer Update.htm Go to my webpage for information! It is pretty much a jounal of my 'Battle wilth Esophageal Cancer'! ALso pictures and anecdotes of my life that I thought about during the time. I am a survivor! I have gone through many of what you have. Never give Up!
0 -
Just finding my new friends!
Hello all....I'm trying to read everyone's questions and suggestions, and while I don't know if I'll post very often, I've already seen some wonderful sugestions! I don't like going over my details with friends...don't want the attention, but I think here-we're all sharing the same questions and many of the symptoms. That said, I would like to respond to Rhonda's original question using my own experience to see if it helps?
Esophogeal cancer and diagnosted almost 2 years ago, and esophogecteomy 21 months ago. Celebrating 2 years healthy around Christmas, I'd say the answer is good (but maybe not the one you want!) Two years later, I am still nowhere near my old normal....but happy with my new normal, if that makes sense? I weighed 200 lbs. prior to finding my 4 cm. tumor, and weigh 142lbs. today. Everyone's personal stories seem to have various stages....but I am beginning to think I'm going to just be lean for the rest of my life, and choosing to celebrate it! I can eat almost normally, but about 1/3 of my prior volume. The only foods I have major issues with are white flower products (bread), as hypoglycemia is perhaps a bit worse now-get shaky and feel brittle a bit more often. So as little sugar as possible has helped me? Also, deyhdration is a major problem. I try to drink 2 liters + of both electrolyte water (cheap drops at Kroger) alternated with Grapefruit juice and tonic water-very refreshing! I too enjoy an evening glass of wine, but as it is a diuretic, go easy....having spent several nights in the hospital for a RIND (reversable stroke brought on by dehydration), I know better...lol A year ago, had an abdomial hernia from the prior surgery, so had to have mesh put in to hold my insides in....another 9 days in the hospital. So with two 9 day hospital stays under my belt....the chemo/radiation/2 big anasthesias have left me a bit "not the sharpest knife in the drawer" anymore...grins.
In my case, physical exertion is very much a wonderful thing-mowing the yard, pulling weeds (don't bend over-you'll find out why if you do....) makes me feel far more solid and steady, which is a blessing. Howver, talking and trying to be "on" for more than an hour at a time totally wipes me out...so we try to put limits on going out to lunch and stuff.
I don't know if I'm helping anyone, but here's a couple of ideas that might help. Find a good wedge pillow....I travel with mine everywhere for sleeping. As for putting weight back on....I have no help...but am taking digestive enzymes plus a handfull of vitamins daily/with every meal. We don't absorb like we used to, which has all the consequences we've identifed on this thread. I've got a friend that is a Gastric Surgeon, and he's got my medical team looking into a "medical food" called Enterogam. It's a bit pricy, but I haven't started on it yet. I should get is soon, and will be the guenny pig for this forum! Warm drinks and room temperature are best.....throat clamps down completely with ice cold. Exercise, sunshine, and always keep snacks close by so you learn your own new normal! Have to put my short evangelical plug in at the end.....God is good, as we are all here talking! I can't imagine having to go through this by myself, I don't think I'd still be around otherwise. Thanks all, and I'll keep checking in!
Dale
0 -
Dale~Glad 2 hear from another EC SURVIVOR~Welcome
Dear Dale:
A sincere welcome from all of us here on the site. I’ve just read back through the responses from the very top, and I can say that anyone who doesn’t know what to expect after their Esophagectomy, no matter the type, would do well to “print out” this page. Then they can check in at intervals, and see if what they’re experiencing is discussed. It certainly is a “new normal”, but we are all glad to be alive. Sad to say, we do have some that write here, and never check back in for the answer. I note by Rhonda’s “about-me page”, that she signed on November 9, 2015, and never posted again after that. So we don’t know the end of her story. But as noted at the bottom of her posting, I see that 12,778 others have read it, so our advice has not “fallen on deaf ears!” We have lots of “lurkers” who read but never join and post anything. That’s okay too. So surely, others have benefitted by what we’ve had to say!
I’m a thankful recipient of God’s grace and mercy, unworthy though I am. He promises to never leave me or forsake me. Long ago I read the little saying, “When God seems far away—guess who moved?” Awareness of His presence carries my husband and me on the many days of uncertainty that all we cancer patients cope with. Finite and fragile creatures we are, but it is my complete trust in an omniscient, omnipresent and omnipotent God that allows me to have peace in my soul, even as my body continues to deteriorate. I am not “out of the woods” but thankful to have lived this long. As a Stage IV terminal cancer patient, one’s goal is to experience as long a “progressive free survival” as possible. My husband, William, aka Bill or Billy, and I both have the same oncologist. Today Bill had his semi-annual checkup, and received another “good-to-go” with no evidence of disease report.
 Talk about a blessing! ! So we’re happy to still have each other. I’m happy to still be around to “tell him what to do” and he’s happy to still be around “to do it!”
Talk about a blessing! ! So we’re happy to still have each other. I’m happy to still be around to “tell him what to do” and he’s happy to still be around “to do it!” 
Cancer certainly makes me, and most likely many of us here, more appreciative of the “little things” that we once seemed to think we were entitled to, like sunshine, air, food, water and good doctors plus being born in America! Close family ties are ever so important. Hugs, phone calls, thinking-of-you cards and letters, prayers and well wishes remind us that we are loved and NEEDED to make someone else’s life complete. Although none of us would have “ordered” this cancer as a “maturing” experience that would ultimately be for our good, I believe that we all have “grown up” even more since being a cancer patient. People are hurting everywhere, and when we can comfort others and show compassion as a result of our own experiences, setbacks and victories, then we feel life is still worthwhile.
As for the “newbies”, it’s always good to learn from others who have already traveled the road we’ve been on. And really, we “veterans” are not on here for our own health, as much as it is that we desire to help others. We remember the shock-and-awe days when we were first diagnosed, as well as the many days of uncertainty, because we knew so little. And now, though none of us pretend to be doctors, collectively we do provide a valuable insight into what the expression, “a new normal” really means.
My husband and I just like to say that “we’re just a couple of beggars telling another beggar where to find a piece of bread.” I think that I can speak for “Paul and Ed” as well. They have been faithful to share their defeats and victories and I appreciate them so. Their contributions to this site are so much appreciated. Thank you for sharing your story. We love hearing from other “survivors”.
Wishing you continued success,
“Two happy beggars”,


Loretta-Stage IV Peritoneal Carcinomatosis/Ovarian Cancer DX Nov. of 2012
& William-15 year survivor - DX Nov. 2002, EC Stage III, (T3N1M0), Adenocarcinoma at the GE Junction, Neoadjuvant chemo/radiation/then MIE at University of Pittsburgh Medical Center performed by Dr. James D. Luketich on May 17, 2003.
0
Discussion Boards
- All Discussion Boards
- 6 CSN Information
- 6 Welcome to CSN
- 122K Cancer specific
- 2.8K Anal Cancer
- 446 Bladder Cancer
- 309 Bone Cancers
- 1.6K Brain Cancer
- 28.5K Breast Cancer
- 398 Childhood Cancers
- 27.9K Colorectal Cancer
- 4.6K Esophageal Cancer
- 1.2K Gynecological Cancers (other than ovarian and uterine)
- 13K Head and Neck Cancer
- 6.4K Kidney Cancer
- 673 Leukemia
- 794 Liver Cancer
- 4.1K Lung Cancer
- 5.1K Lymphoma (Hodgkin and Non-Hodgkin)
- 238 Multiple Myeloma
- 7.2K Ovarian Cancer
- 63 Pancreatic Cancer
- 487 Peritoneal Cancer
- 5.5K Prostate Cancer
- 1.2K Rare and Other Cancers
- 543 Sarcoma
- 736 Skin Cancer
- 657 Stomach Cancer
- 192 Testicular Cancer
- 1.5K Thyroid Cancer
- 5.9K Uterine/Endometrial Cancer
- 6.3K Lifestyle Discussion Boards




