Omentum surgery/removal questions
Hi all, I had hoped to get thru the holidays before tackling this topic, but my abdomin doesn't look "right" and the CT in August showed cancer in the omentum fat. I want to explore surgerry. Have not had any surgerry since diagnosis in May via laproscopic. Surgeon said could not do surgery, would have to do chemo.
Taxol/carbo worked great until infection. Now on 3 weeks on Abraxane (paclitaxel) with Avastin added to week one only. Then one week off. There is a buldge at my waistline, right side--new. Thinking it is the omentum???
Julie, Carole, Nadine, and anyone else I need info. Cannot remember who has had the surgery, but would really appreciate anything you can add on the omentum surgery topic for me. Will have the discussion with onc in January.
Flying solo to have Christmas with daughtergrandson on Tues the 24th with hubby joining for weekend after new year. We didn't want daughter to be alone for holiday since ex gets grandson for Christmas eve and day. First time.
Blessings of the season to all--I count all of you as blessings--thank you!!!
Sue
Comments
-
My questions--omentum surgerryabrub said:My omentum was completely removed
It had no effect on my lifestyle. There was cancer seeded throughout it, so my surgeon removed it. It isn't a major organ, just a protective fat layer. What is your question/concern?
Arub--thanks for the response! Hope December is being kind to you, we are in the midst of ice drizzle.
Alexandra--if you read this --as soon as I submitted my request, I saw that I did not include you, and you and the others have had such great posts. Please add too. I lam sure I have left someone off and could not remember who had surgery--my brain is toast.
Questions: Length hospital stay, length of recovery at home ie how long before driving? Chemo sschedule during this perriod, what do wbc numbers need to be to have the surgery. I am told most have this with debulking before chemo--missed that boat. What pain reliever worked for you? Are there choices I will be given by the surgeon?
My oncologist's nurse said no one in my home city is willing to do the procedure, so patients are referred to our Nebraska Medical Centerr in Omaha. I had a consult there for my infection in October and they are great! It was on my radar to get surgery/ca consult there during the new year. I trust my onc totally--he was my onc 15 years ago--
I know i will think of more questions--please bombard me with details.
Thanks and blllessings to all, Sue
0 -
Omentum surgerysk_Nebraska said:My questions--omentum surgerry
Arub--thanks for the response! Hope December is being kind to you, we are in the midst of ice drizzle.
Alexandra--if you read this --as soon as I submitted my request, I saw that I did not include you, and you and the others have had such great posts. Please add too. I lam sure I have left someone off and could not remember who had surgery--my brain is toast.
Questions: Length hospital stay, length of recovery at home ie how long before driving? Chemo sschedule during this perriod, what do wbc numbers need to be to have the surgery. I am told most have this with debulking before chemo--missed that boat. What pain reliever worked for you? Are there choices I will be given by the surgeon?
My oncologist's nurse said no one in my home city is willing to do the procedure, so patients are referred to our Nebraska Medical Centerr in Omaha. I had a consult there for my infection in October and they are great! It was on my radar to get surgery/ca consult there during the new year. I trust my onc totally--he was my onc 15 years ago--
I know i will think of more questions--please bombard me with details.
Thanks and blllessings to all, Sue
Hi Sue
I too had my omentum removed as part of debulking surgery following 4 cycles of carbo/taxol. Like Abrub's it was seeded with microscopic cancers and I have not had any problems or difficulties without it. This was done in March 2012. I was in hospital for about 10-12 days and had painkillers via epidural - amazing result for me. I started back on carbo/taxol approx 3 weeks later. I can't recall how long before I drove but think probably 6-8 weeks following surgery.
Enjoy your Christmas with your daughter.
Julie
0 -
Thanks for reply
Julie and arub, thanks for the information. I am amazed that both of you had such positive comments. The surgeons here are almost afraid to tackle. maybe because they would be general surgeons. My youngest daughteer is a pediatrician and she was very pessimistic about the ability to remove omentum. Kids and adults are soooooo different and she seems to interact with the most critical--hospitalist at a major childrens hospital , so I take some things with a " so anxious to get it gone! My ca125 at diagnosis was in the 5 digits--sure due to no surgery. With the BC had masectomey prior to chemo--onc not happy, but Im glad i did it that way.
Thanks for the info. Are there any complications I should know about? CONSTIPATION has given me the incentive to invest in MiraLax:)
Sue
0 -
Omentum surgerysk_Nebraska said:Thanks for reply
Julie and arub, thanks for the information. I am amazed that both of you had such positive comments. The surgeons here are almost afraid to tackle. maybe because they would be general surgeons. My youngest daughteer is a pediatrician and she was very pessimistic about the ability to remove omentum. Kids and adults are soooooo different and she seems to interact with the most critical--hospitalist at a major childrens hospital , so I take some things with a " so anxious to get it gone! My ca125 at diagnosis was in the 5 digits--sure due to no surgery. With the BC had masectomey prior to chemo--onc not happy, but Im glad i did it that way.
Thanks for the info. Are there any complications I should know about? CONSTIPATION has given me the incentive to invest in MiraLax:)
Sue
Hi Sue
My surgery was done by a gyne-oncologist not a general surgeon. I didn't have any complications - re constipation I am fortunate probably that my large bowel was removed when I was in my 20's so that is something that doesn't trouble me so I can't advise on that point.
Cheers, Julie
0 -
Surgery
Hi Sue,
I too like Julie had my debulking surgery prior to my chemo with everything being removed at that time. I was full of disease and was in a 51/2 surgery. I was in the hosiptal for 8 days one day including my portacath being put in. I flew from North Carolina to Texas for a second opinion when I had recovered for 5 weeks. They wanted to start my chemo at 3 weeks after surgery but I went to get a second opinion. I wasn't suppose to drive until 6 to 8 weeks but I drove to my work in 5 weeks. I healed really well and fast. Good luck to you and if you have any more questions I will be happy to answer. Praying for you.
Merry Christmas to you and your family!
Nadine
0 -
Still have my omentum--I think.
I did not have omentum removed--so far as I know! (I should know, & I'll fix that. I still have a nice flap of tummy flab, so I assume the omentum is still there.) Upon my diagnosis I went straight to chemo. I've always thought that was because 4 yrs before, I had a complete hysterectomy including ovaries. Upon completion of my 1st chemo course in Dec. 2012, surgery was recommended. I was told it was because it wasn't entirely clear via scans, etc., what remained in my peritoneum. PET scan in Sept. 2012 showed great decrease in largest tumors & complete absence of others; PET scan in Dec. 2012 showed not that much more change.
Before surgery the medical advice was that what remained was likely mere scar tissue, but could be cancerous. So upon completion of surgery in Feb. 2013, gynecological oncology surgeon said no visible cancer; unfortunately, a week or so later 3 of 6 biopsies were still positive for cancer. That's why I embarked on more chemo in March 2013; just finished it all this week. I was supposed to go home the same day as surgery, but the doc decided to keep me overnight because my oxygen level was a little low. Surgery was hoped to be laparascopic; turned out he made a small incision above my navel. I don't remember much about pain, except having those abdominal muscles cut took some time for recovery.
Unfortunately, my CA 125 has been rising steadily since last summer, tho in Sept I was declared "no evidence of disease." I have found these references:
- "High values of CA-125 in a woman who has been treated for ovarian cancer may mean that the cancer has returned. Often the high CA-125 level is found many months before the return of cancer can be found in another way."--WebMD
- "Among patients in complete clinical remission, a progressive low-level increase in serum CA-125 levels is strongly predictive of disease recurrence."--Journal of Clinical Oncology
The last describes me precisely, & my CA 125 is now out of the normal range. My oncologist says he can't find anything by palpating my abdomen. I go in for a CT scan on New Year's Eve and a few days later will hear what is recommended next. I will not be surprised to be told my cancer has recurred. As always, details are at www.CaringBridge.org/visit/CaroleSeaton/journal
Good luck! Enjoy your holiday with family. Sorry I can't be more help except to provide my own experience. . . .
0 -
debulking surgeryNflinchum said:Surgery
Hi Sue,
I too like Julie had my debulking surgery prior to my chemo with everything being removed at that time. I was full of disease and was in a 51/2 surgery. I was in the hosiptal for 8 days one day including my portacath being put in. I flew from North Carolina to Texas for a second opinion when I had recovered for 5 weeks. They wanted to start my chemo at 3 weeks after surgery but I went to get a second opinion. I wasn't suppose to drive until 6 to 8 weeks but I drove to my work in 5 weeks. I healed really well and fast. Good luck to you and if you have any more questions I will be happy to answer. Praying for you.
Merry Christmas to you and your family!
Nadine
Hi Sue - I was dioagnosed Spring 2013 - late diagnosis as most - alllowing time for cancer to metasticize to organs in the abdominal cavity.
I took 2 rounds of 6 chemo treatments with carboi/ taxol to shrink the mets canc er before surgery--- it is more successful the smaller the tumors - figured they knew best.
I see a gyne/onc who difd the surgery on Oct 29 & was very pleased with the results
I was in the hosp about 10 days - I have other medical problems pain was addressed with a "happy button" morphine on demand with a set limit.
All in all I can't say pain was a huge problem
avg recovery time is 6-8 weeks with nno heavy lifting for 3 mos. I had no complications or real problems
I was both excited & scared 5to get a date excited - to be doing something positive in the fight scarecd- of the unknown
wqe live in a small agriculture town & have to travel 2 hrs ea way for my cancer care & surgery
best wishes
SusanP
0 -
You want a specialist to do the surgerysk_Nebraska said:My questions--omentum surgerry
Arub--thanks for the response! Hope December is being kind to you, we are in the midst of ice drizzle.
Alexandra--if you read this --as soon as I submitted my request, I saw that I did not include you, and you and the others have had such great posts. Please add too. I lam sure I have left someone off and could not remember who had surgery--my brain is toast.
Questions: Length hospital stay, length of recovery at home ie how long before driving? Chemo sschedule during this perriod, what do wbc numbers need to be to have the surgery. I am told most have this with debulking before chemo--missed that boat. What pain reliever worked for you? Are there choices I will be given by the surgeon?
My oncologist's nurse said no one in my home city is willing to do the procedure, so patients are referred to our Nebraska Medical Centerr in Omaha. I had a consult there for my infection in October and they are great! It was on my radar to get surgery/ca consult there during the new year. I trust my onc totally--he was my onc 15 years ago--
I know i will think of more questions--please bombard me with details.
Thanks and blllessings to all, Sue
Mine was done by a colorectal surgical oncologist, but in my case, the peritoneal cancer was mets from my appendix cancer. I had a specialist surgeon, and then followed with IntraPeritoneal chemo, but again, based on a colorectal cancer.
(Side note - even without my omentum, I've managed to put on substantial belly flab. I gained lots of weight post chemo.)
Alice
0 -
Hi Sue,sk_Nebraska said:My questions--omentum surgerry
Arub--thanks for the response! Hope December is being kind to you, we are in the midst of ice drizzle.
Alexandra--if you read this --as soon as I submitted my request, I saw that I did not include you, and you and the others have had such great posts. Please add too. I lam sure I have left someone off and could not remember who had surgery--my brain is toast.
Questions: Length hospital stay, length of recovery at home ie how long before driving? Chemo sschedule during this perriod, what do wbc numbers need to be to have the surgery. I am told most have this with debulking before chemo--missed that boat. What pain reliever worked for you? Are there choices I will be given by the surgeon?
My oncologist's nurse said no one in my home city is willing to do the procedure, so patients are referred to our Nebraska Medical Centerr in Omaha. I had a consult there for my infection in October and they are great! It was on my radar to get surgery/ca consult there during the new year. I trust my onc totally--he was my onc 15 years ago--
I know i will think of more questions--please bombard me with details.
Thanks and blllessings to all, Sue
i am new to thisHi Sue,
i am new to this board and new to this disease. i found out on Dec 11, 2013 that my pap had cancer cells and it's been a whirlwind since. I had a ct scan that showed growths in my omentum so I had it removed along with all my female parts on Jan 6. I'm still recovering from this and we are trying to set up my chemo. I am waiting to hear if I will be involved in a clinical trial with Avistin and a new PARP inhibitor. Until then, it's just waiting. I wanted to answer your questions, in case you haven't had the surgery yet.
My actual surgery was about 2 or so hours since there wasn't visible cancer anywhere but on my omentum. They will check many organs to make sure cancer isn't lurking and will remove when found. They did a wash of my area and found microscopic cancer cells.
I was in the hospital for 2 nights. My surgery began at 4 pm and I don't remember much of that day. I was on an IV and had a catheter so I didn't need to do much. The next day I had pain and loved my Percocet and prescription Motrin. I was up and walking that day and I left the hospital the next day.
I drove for the first time a few days ago and feel better every day. The first week I pretty much layer on my recliner and didn't leave except to go to the bathroom. Eating is challenging because elimination is challenging. I resorted to taking dulcolax which helped.
I took the extra strength prescription Motrin and the Percocet for the first few weeks. They didn't give me choices but these worked well for me. I am doing just fine without my omentum, I don't notice a change in how my body looks or feels.
I have so many questions about what to expect with chemo. I'll be on carob and taxol and maybe the 2 additions. I have kids at home so am trying to keep positive for them.
I wish you all the best luck fighting this rare cancer.
Michelle
0 -
Michelle--Chemo questions
Chemo will be different but not unmanageable, Start the anti nauseau Zofran the night of your first chemo. You wont have nausea until probably mid day 2 but good to get it controlled. My nausea usually was gone by late day 3. Took compazine in between after that,.If you get ahead of it you won't have it. Besure to drink minimum 8 glasses of water daily--flush kidneys. Get a reliable laxative on hand. Miralax powder works for me. Twice daily. Stock up on Poise pads, Serenity (depends) just in case. Also wet wipes for clean up. Keep up the hygeine. I got a used diaperr genie for those unplanned monents. Goold luck.I am meetin with surgeon for hot chemo surgery consult. Will have lots of questions for you then.
Hang in there. Get on an antidepressant if you need to!! I hooked up with a nurse navigator thru the ACS who acted as a councelor when I had bc.Shewas great.
Good Luck!!!!!
Sue
0 -
Omentum Removal
Hi all,
I know it has been a while since this chat has been active, but I was hoping some of you were still on here. My father has cancer that spread to his omentum and I wanted to see where I could find more informaiton. He is concerned with recovery after removal and the extensivness of the surgery. Could you point me in the direction of where to learn more about this, I am having trouble finding anything on Google?
Thank you!
Erich
0 -
Erich~A few links re info about the Omentum & Peritoneum
Dear Erich –
It would have helped if you had told us the original diagnosis of your dad. I too had cancer that had spread to the omentum. More than one type of cancer can metastasize to the omentum. Both gastrointestinal and gynecological cancers can spread to the omentum. In my case, my very first diagnosis by CT scan was correct. It was “Peritoneal Carcinomatosis”. A second opinion at UPMC in Pittsburgh also found it to be in my ovaries as well. Primary peritoneal cancers are rare as compared to cancers that have spread to the peritoneal cavity from another organ.
In my case my Stage IV diagnosis probably originated in the ovaries and then spread to the Peritoneum. I knew one young man who had Peritoneal Carcinomatosis that resulted from his appendix rupturing. Other cancers like stomach and colorectal cancers can also spread to the Peritoneum. In my case I had “multiple tumors” floating around in the peritoneal fluid in my abdominal cavity. Resultant therapy included first a series of Carboplatin/Paclitaxel chemotherapy regimen consisting of 6 treatments, each 3 weeks apart. Then Cytoreductive Surgery (though never intended to be curative) was performed July 1, 2013 at the University of Pittsburgh Medical Center. There Dr. David Bartlett removed my ovaries, fallopian tubes, gallbladder, spleen, omentum and sections of my intestines. When I first was diagnosed, the heated intraperitoneal chemo (HIPEC) procedure was discussed as a possibility during my surgery, but the doctor decided against it once surgery had begun.
So my suggestion is that you key in the words, Peritoneum, Omentum, and HIPEC for starters as well as whatever your dad’s original diagnosis was. Many articles are filled with medical terminology that I, as a layman, don’t understand, but I ask my oncologist lots of questions, and sometimes print out the article, take it to him, and ask for an explanation.
But Erich, since I really don’t know where to begin with you, I have listed some references below that will give you a starting point. I do hope that your dad has had a 2nd opinion, and that he will be being treated at a major medical facility.
Since my husband has a garden every year, and often uses “Miracle Grow” to hasten and enlarge the fruit, flowers or vegetables, if you think of that as a comparison, the omentum is considered very fertile hotbed and tumors thrive there very well. I know that information on Peritoneal Carcinomatosis is not as easily researched as some other cancers.
The Lord has blessed me to be able to survive for 5 years after my diagnosis and for that I am so thankful. So while my cancer isn’t curative, there are treatments that can allow me to still have some “quality life” in between. The treatments aren’t fun, but tolerable so far, although I am running out of options. But I always have to say, as a Christian, I firmly believe the truths laid out in Psalm 139 and am firmly convinced that my times are in God’s hands. He alone knows the number of my days. It is my responsibility to find the very best doctors who will be honest and tell me the truth. So I always have to say, I will not live one day longer or die one day sooner than my allotted number of days here. Understand though there is no one that wants to leave their beloved family and friends, but after all we are mortal. So my prayer for your dad would be that whatever his exact diagnosis happens to be is that he will find some good treatments and experience a long and good quality of life.
Loretta – Peritoneal Carcinomatosis/Ovarian Cancer Stage IV, DX Nov. 2012
_______________________________________________________________
Note: These first two references are videos describing just where the peritoneum is and what is the lesser and greater omentum. If you find them too difficult to be of any help, just skip over them. But I never knew anything about the Peritoneum until I had been diagnosed with Peritoneal Carcinomatosis. I have to listen and look at this over and over in order to begin to understand the different parts of my abdominal cavity. But the doctor uses these words freely, naturally, and I see them on my scans, so the more familiar I become with them, the better I understand how the Lord put me together!
1.
 https://www.youtube.com/watch?v=4yvjIFcB4h4
https://www.youtube.com/watch?v=4yvjIFcB4h4Greater and lesser omentum explained
_________________________________________________
2.
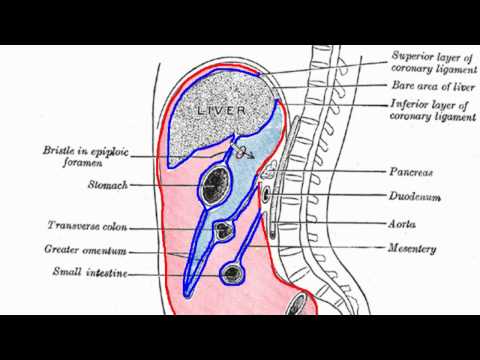 https://www.youtube.com/watch?v=Uo3jDAXR_Ww
https://www.youtube.com/watch?v=Uo3jDAXR_WwPeritoneal Cavity - Part 1 - Anatomy Tutorial
_____________________________________________
3. https://www.mskcc.org/clinical-updates/targeting-peritoneal-cancer-metastases
Targeting Peritoneal Cancer Metastases
By Garrett M. Nash, MD, MPH, FACS, FASCRS,
Thursday, May 19, 2016
“Over the past 15 years, Memorial Sloan Kettering Cancer Center (MSK) and other specialty centers have been treating patients with peritoneal spread of appendix and colorectal cancer. Treatment includes debulking or cytoreductive surgery (CRS) to remove all visible tumor, followed by intraperitoneal chemotherapy (IPC), the delivery of chemotherapy directly into the abdomen to attempt to eliminate the microscopic disease that may remain after surgery.1 Using this approach, patients with appendix cancer have better long-term survival — some with more than 10 years — than some patients with other stage IV cancers. 2 colorectal cancer with peritoneal metastasis, however, is a more challenging problem; despite the most aggressive surgery and chemotherapy available, there are few cures…”
______________________________________________________________
4. https://emedicine.medscape.com/article/193622-overview
“Solid Omental Tumors
Updated: Sep 05, 2017 - Author: Kendrix J Evans, MD, MS; Chief Editor: John Geibel, MD, DSc, MSc, AGAF more...
Overview Background Anatomy Pathophysiology
- Epidemiology Prognosis Show AllPresentation DDx
- Workup Treatment Media Gallery Tables References
Background
Metastatic tumors of the omentum are common.
In contrast, primary tumors of the omentum are very rare, [1] and the etiologic agents responsible for causing them are unknown.
Stout and Cassel described the first reported case of a primary omental tumor in 1942. The patient had a 60-year history of a palpable abdominal mass before dying of heart failure at age 92 years. An omental hemangiopericytoma was identified at autopsy.
Complete surgical excision offers the best chance of cure. The role of adjuvant therapy in the management of malignant omental tumors is uncertain. Because of the rarity of these lesions, the effectiveness of chemotherapy and radiation therapy has not been established. Advances in these treatment modalities may improve future survival rates for patients with malignant primary omental tumors…”
_________________________________________________
5. http://www.cancertherapyadvisor.com/gastrointestinal-cancers/colorectal-cancer-peritoneal-carcinomatosis-treatment-options/article/408012/
“Treatment Options for Peritoneal Carcinomatosis Associated with Colorectal Cancer
As newer treatment options for peritoneal carcinomatosis are developed, more clinical data is needed to support use in patients with colorectal cancer.
Peritoneal carcinomatosis (PC) is one of the most serious complications of gastrointestinal and gynecological malignancies.
The peritoneum is the lining within the abdominal cavity and covers the intra-abdominal organs. It has several components including the outer (parietal) and inner (visceral) layers as well as the greater and lesser omentum.
The peritoneum supports the structure and metabolism of the intra-abdominal organs by providing an important source of blood and lymph circulation. The peritoneum therefore has a significant immunological role in localizing and attacking certain infections.
As the peritoneum is a relatively vascular and lymphoid structure, it can be a potential site of metastases from numerous malignancies, which leads to the diagnosis of PC.
There are several proposed mechanisms of how patients can develop PC. There can be direct extension of the intra-abdominal malignancy into the peritoneum or direct seeding of the peritoneum following tumor rupture.1
The peritoneum can also be seeded during surgery, especially when the abdomen is exposed to the contents of the lymph nodes or blood vessels during surgical exploration.
The clinical data are somewhat variable, however this direct seeding during potentially curative surgeries has been reported to be between 3% and 28%.1
RELATED: Almost Half of Colorectal Cancer Survivors Experience Continued Pain
It may be extremely difficult to ascertain when the peritoneum is seeded with malignant cells, as there may be a minute amount of cells that remain relatively undetectable by conventional means. PC has been reported in up to 40% of patients with colorectal cancer (CRC) at any time point within their clinical course.2
Treatment of PC can vary based on the site of the primary malignancy. Most of the recent data and clinical trials have focused on PC associated with CRC.
Older, more traditional treatments in patients with PC secondary to CRC include removal of the omentum, systemic and/or palliative chemotherapy, and palliative surgery. Newer treatment options include cytoreductive surgery (CRS), hyperthermic intraperitoneal chemotherapy (HIPEC), and intraperitoneal chemotherapy.
Traditionally, PC secondary to ovarian cancer has been more responsive to chemotherapy than PC secondary to CRC, however these newer treatment modalities have provided some hope in the form of prolonged survival.1,2
Older systemic chemotherapy regimens such as 5-flurouracil (5FU) and leucovorin provided a limited survival benefit of around 7 months while additional agents like oxaliplatin and irinotecan were able to extend survival to approximately 23 months.2
The newer treatment regimens (CRS and HIPEC) have shown survival benefit of up to 63 months with a 5-year survival near 50%.2
There are several scales that rate the extent of PC and provide a prognostic estimate that can help stratify patients for potential treatments.
These scales include the Peritoneal Cancer Index (PCI) and the Peritoneal Surface Disease Severity Score (PSDSS). The scales can include information regarding the patient's symptoms as well as the location and size of the patient's PC tumor burden.2,3
Certain patients who have a poor prognosis based on these scales may not be the ideal candidates for more aggressive surgery or chemotherapy.2
For example, the 5-year survival rates of patients with CRC who have PC based on the PCI include: 50% with PCI 10 or less, 20% with PCI of 11 to 20, and 0% with PCI more than 20.3
Therefore, patients with a PCI of more than 20 are typically not considered candidates for the newer, more aggressive therapies.
RELATED: Women Overweight in Youth May Face Higher Colorectal Cancer Risk
Many patients with extensive liver metastases and intra-abdominal lymphadenopathy may also be considered to have relative or absolute contraindications to the newer treatments secondary to poor prognosis.
As with many of the new and upcoming oncology treatments, additional clinical data is needed to continue to support the use of newer treatment options in PC associated with CRC.
These newer options, such as cytoreductive surgery and HIPEC, may provide a certain subgroup of patients with PC an additional survival benefit that they were not candidates for…”
__________________________________________________________
6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1780209/
“Preferential Attachment of Peritoneal Tumor Metastases to Omental Immune Aggregates and Possible Role of a Unique Vascular Microenvironment in Metastatic Survival and Growth
Abstract
Controlling metastases remains a critical problem in cancer biology. Within the peritoneal cavity, omental tissue is a common site for metastatic disease arising from intraperitoneal tumors; however, it is unknown why this tissue is so favorable for metastatic tumor growth. Using five different tumor cell lines in three different strains of mice, we found that the omentum was a major site of metastases growth for intraperitoneal tumors. Furthermore, initial attachment and subsequent growth were limited to specific sites within the omentum, consisting of organized aggregates of immune cells. These immune aggregates contained a complex network of capillaries exhibiting a high vascular density, which appear to contribute to the survival of metastatic cells. We found that the vasculature within these aggregates contained CD105+vessels and vascular sprouts, both indicators of active angiogenesis. A subset of mesothelial cells situated atop the immune aggregates was found to be hypoxic, and a similar proportion was observed to secrete vascular endothelial growth factor-A. These data provide a physiological mechanism by which metastatic tumor cells preferentially grow at sites rich in proangiogenic vessels, apparently stimulated by angiogenic factors produced by mesothelial cells. These sites provide metastatic cells with a microenvironment highly conducive to survival and subsequent growth.
Controlling metastases remains a critical problem in cancer biology. Within the peritoneal cavity, omental tissue is a common site for metastatic disease arising from intraperitoneal tumors; however, it is unknown why this tissue is so favorable for metastatic tumor growth. Using five different tumor cell lines in three different strains of mice, we found that the omentum was a major site of metastases growth for intraperitoneal tumors. Furthermore, initial attachment and subsequent growth were limited to specific sites within the omentum, consisting of organized aggregates of immune cells. These immune aggregates contained a complex network of capillaries exhibiting a high vascular density, which appear to contribute to the survival of metastatic cells. We found that the vasculature within these aggregates contained CD105+vessels and vascular sprouts, both indicators of active angiogenesis. A subset of mesothelial cells situated atop the immune aggregates was found to be hypoxic, and a similar proportion was observed to secrete vascular endothelial growth factor-A. These data provide a physiological mechanism by which metastatic tumor cells preferentially grow at sites rich in proangiogenic vessels, apparently stimulated by angiogenic factors produced by mesothelial cells. These sites provide metastatic cells with a microenvironment highly conducive to survival and subsequent growth.
Malignant cells often metastasize into the peritoneal cavity from intra-abdominal primary tumors including ovarian, colon, and stomach.1–3 For these intra-abdominal tumors, direct intraperitoneal seeding is a common avenue of metastatic dissemination, although lymphatic and hematogenous spread can also occur. This direct seeding can arise when tumor cells are dislodged from the primary neoplasm, either naturally or during the process of surgical tumor resection, and the natural flow of peritoneal fluid then transports these malignant cells throughout the abdomen.2,4 This metastatic stage of disease is frequently characterized by aggressive tumor growth resulting in a poor prognosis…”
__________________________________________________________
7. https://www.ncbi.nlm.nih.gov/pubmed/26831659
“Abstract - Tumour Biol. 2016 May;37(5):5715-26. doi: 10.1007/s13277-016-4887-3. Epub 2016 Jan 29.
Milky spots: omental functional units and hotbeds for peritoneal cancer metastasis.
Liu J1, Geng X1, Li Y2,3. Author information Abstract
As the most common metastatic disease of abdomen pelvic cavity cancer, peritoneal carcinomatosis (PC) renders significant negative impact on patient survival and quality of life. Invasive peritoneal exfoliated cancer cells (PECCs) preferentially select the omentum as a predominant target site for cancer cell colonization and proliferation compared with other tissues in the abdominal cavity. The precise pathogenic mechanism remains to be determined. As omental milky spots (MSs) are the major implantation site for malignant cells in peritoneal dissemination, researches on mechanisms of PC have been mainly focused on MS, primitive lymphoid tissues with unique structural features, and functional characteristics. To date, extensive biophysical and biochemical methods have been manipulated to investigate the MS exact function in the peritoneal cavity. This review summarized MS as hotbeds for PECC. The anatomical distribution was briefly described first. Then, MS histology was systematically reviewed, including morphological features, cellular constituents, and histological staining methods. At last, the roles of MS in PC pathological process were summarized with special emphasis on the distinct roles of macrophages.
KEYWORDS:
Cancer; Invasion and metastasis; Omental milky spots; Peritoneal carcinomatosis”
________________________End of references_________________
0 -
Omentum Removal
Hi. I had my omentum removed in 2013. I dont have a great understanding as to why. I will explain what i do understand. I had gotten really sick, to where my stomach had swelled up to a person that looked about 6 months pregnant. Mind you i was not pregnant, and i weighed aprox 125 pounds. However, i took the pain and discomfort for about a week until my boss decided to take me to the emergency room herself. (I never called in sick) Anywho, after about an hour of some testing, i was put in a chair and taken into the ICU. They were giving me all sorts of antibiotics through my veins, and somehow it made it worse. So after about 13 days, i was taken up to the "Cancer floor". Was their for another 10 days. All kinds of specialists would go by, poke me, and explain what they were their for. So once all of the different specialists were able to gather to perform some sort of a surgery where 6 different encisions were to be made with a microscope inserted to see what was causing this huge inflamation in and around the Omentum. Please Note: I was not told that anything was going to be removed. So to my surprise when i wake up, i scream in intense pain, and was informed that they removed my omentum because it was full of an infection that to this day, i have no idea what caused it. My reason for joining this site is to ask if anyone has had any pain in that area after the fact. Other than the initial recovery time. I find myself having to take 2 aleve to ease the pain atleast 3 times a week now. PLEASE forgive my non-saavy way of explaining.
0
Discussion Boards
- All Discussion Boards
- 6 CSN Information
- 6 Welcome to CSN
- 122K Cancer specific
- 2.8K Anal Cancer
- 446 Bladder Cancer
- 309 Bone Cancers
- 1.6K Brain Cancer
- 28.5K Breast Cancer
- 398 Childhood Cancers
- 27.9K Colorectal Cancer
- 4.6K Esophageal Cancer
- 1.2K Gynecological Cancers (other than ovarian and uterine)
- 13K Head and Neck Cancer
- 6.4K Kidney Cancer
- 673 Leukemia
- 794 Liver Cancer
- 4.1K Lung Cancer
- 5.1K Lymphoma (Hodgkin and Non-Hodgkin)
- 239 Multiple Myeloma
- 7.2K Ovarian Cancer
- 65 Pancreatic Cancer
- 487 Peritoneal Cancer
- 5.5K Prostate Cancer
- 1.2K Rare and Other Cancers
- 543 Sarcoma
- 737 Skin Cancer
- 657 Stomach Cancer
- 192 Testicular Cancer
- 1.5K Thyroid Cancer
- 5.9K Uterine/Endometrial Cancer
- 6.3K Lifestyle Discussion Boards




