Radical Prostatectomy - in depth questions
1. What is PLND?
I've read that it relates to lymph nodes test, but could't find if it's something that is done during the surgery or after?
And what does this test mean? how accurate is it?
Is it being done on every surgery or is it according to surgeon decision?
2. Does in every open Radical Prostatectomy the patient needs blood?
How the surgeon decides whether to give blood?
3. Is there only one surgeon performing the surgery, or does he have any assistant (besides the anesthetic, nurse)?
I mean - does the actual surgery is performed by one surgeon or more?
4. What is the average recovery time which the patent is able to walk by himself without pain?
5. How accurate is the post surgery pathology report in predicting the recurrence of the tumor?
6. According to what the surgeon decides whether to do the nerve sparing??
Does he decides before surgery or after?
Thank you all for your support and informative help !!
Comments
-
Perineum, you should find answers in your doctor's office too
Hi Perineum,
I read your post in another forum, but you should find answers in your doctor's office too. A second opinion from an oncologist is always recommended, particularly in high risk cases (Gs 8).
To answer your first question;
PLND stands for pelvic lymph node dissection. This is a procedure most of urologists use to verify metastasis at the nodes. A series of nodes from the pelvic, are removed and analyzed under a microscope by a pathologist. The procedure can be done alone, before any treatment, for diagnosis purposes (laparoscopic) or it can make part of the surgery procedure.
PLND, however, is not recommended by the NCCN guidelines for low risk cases (PSA ≤10 ng/ml, Gleason score 6, cT1c/T2a). In that contrast, high risk cases (PSA>10, Gleason score 8,9 T3/T4) are usually not recommended for surgery, which would make laparoscopic a tool for diagnosis only.
Nevertheless, some Gleason score 8 patients are recommended for surgery and in such cases, extended PLND is done as santdard. Look at this; http://www.renalandurologynews.com/extensive-plnd-may-improve-prostate-cancer-outcomes/article/202919/
Intermediate cases, Gleason score 7, fall into a group that surgeons take other relevant data to consider PLND, such as PSA density and biopsy core involvement. Particularly if such case is recommended for radiotherapy (as prime or as salvage treatment) where proper lymph node involvement diagnosis is needed to determine the radiation field.
There are also preoperative nomograms to predict lymph node involvement, which is used in some instituitions based on PSA, biopsy Gleason score, and clinical stage. This means that guys falling into the low percentage risk would not be subjected to PLND.
http://www.eu-acme.org/europeanurology/upload_articles/Briganti June PP.pdf
In surgery, before cutting off the prostate gland, some surgeons dissect few lymph nodes firstly and wait for the instant analysis results from the laboratory of the hospital. If cancer is found to exist then the doctor stops the operation because they consider surgery not the proper treatment due to the presence of metastases.
On the other way, many doctors just do the surgery and complete pelvic lymph node dissection and get a total pathological analysis on the parts removed.
In my case (PSA=24.2, Gs=5, T2b), the doctor removed 9 nodes during PLND, sent them to analysis and waited. All the nodes were negative so that he continued the operation.
It should be noted that, there are reported cases (maybe mine as one of them) where negative nodes have been found to harbor occult micrometastases, which leads to biochemical recurrence after RP/PLND or even radiotherapy.
Question 2;
Transfusion is always required in surgery of the prostate. Many vessels are cut and a proper blood supply is needed. In my case, I gave 800cc (2x400) of my own blood one month in advance. That would avoid mismatches or other complications.
Question 3;
In my surgery the team consisted of 5 doctors including the anesthetist. The surgeon was assisted by three doctors (second surgeon and two assistant young doctors for stitches, medication, etc). The whole operation took over 5 hours.
Question 4;
The time to recovery varies from patient to patient. Many report being in recovery (in bed) 24 hours. In my case, the surgery ended at 6pm, awake at 10pm, and was walking 10am on the next day with the help of a tripod (and medicine of course).
From day two I was walking along the corridors of the hospital. It helps in the heeling process and it feels good.
Question 5;
There is lots of controversy regarding nomograms to predict recurrency from a pathological report after surgery. However, all recommendations are based on findings from past cases so that we should assume it correct. Salvage treatments are all based on those statistic data. Unfortunately, the “Silver Bullet” to kill cancer does not exist yet.
In recent studies, genes have been identified in cases of recurrence. The PITX2 gene was associated with cancer recurrence in cases where the prostate has been removed. A test named “hyper-methylation of PITX2 gene” was found accurate in predicting recurrence in cases with organ-confined and non-organ-confined disease.
You can read about details by using a net search engine and typing its name.
http://blue.regence.com/trgmedpol/lab/lab61.html
Question 6;
Nerve spare procedure is decided before surgery. We have to agree (yes or no) and sign the “contract” (my wife signed for radical). However, in a case where nerve spare has been judged to be valid before surgery (by diagnosis), and found to be in “bad-shape” while in surgery, the surgeon may change procedure and remove it without a word (we will be sleeping).
Wishing my insight is of help.
VGama0 -
Open Surgery
Welcome and I'm sorry that you find yourself in the position of needing to ask these questions. VGama did his usual wonderful job in answering your questions-he is a terrific resource. I'll add from my own experience. I had open surgery with lymph node dissection on 3/1/11.
1. I had the dissection during my surgery because I had a suspicious lymph node. My surgeon (William Ellis, Seattle Cancer Care Alliance)did not stop the surgery waiting for the result, but did send the suspicious node if for a quich pathological check.
2. I did not need blood nor was it expected that I would. Dr Ellis told me that it used to be common to need a transfusion but now is much less so.
3. 3 surgeons and 6 hours.
4. I was up walking the next morning. I spent 2 nights in the hospital and pain was never really a problem. I had some, but you get enough pain medication to help. I was walking a mile plus by week 3.
5. That's always the big question. I had the nomograms and all the reports and studies, but "your mileage may vary." A recurrence could always happen, even years later.
6. My surgeon told me before the surgery that he would be able to spare 1 nerve but probably not the other. That is how it turned out. 3 months later I am down to one pad for security only--no real leakage--and partial erections. Still working on that part.
I would recommend Dr Peter Scardino's Prostate Book (the new 2010 revision). It is very helpful. There are also a number of other good books and resources out there. Good luck on your path.0 -
Thank you all for your valuable informationSeattleJ said:Open Surgery
Welcome and I'm sorry that you find yourself in the position of needing to ask these questions. VGama did his usual wonderful job in answering your questions-he is a terrific resource. I'll add from my own experience. I had open surgery with lymph node dissection on 3/1/11.
1. I had the dissection during my surgery because I had a suspicious lymph node. My surgeon (William Ellis, Seattle Cancer Care Alliance)did not stop the surgery waiting for the result, but did send the suspicious node if for a quich pathological check.
2. I did not need blood nor was it expected that I would. Dr Ellis told me that it used to be common to need a transfusion but now is much less so.
3. 3 surgeons and 6 hours.
4. I was up walking the next morning. I spent 2 nights in the hospital and pain was never really a problem. I had some, but you get enough pain medication to help. I was walking a mile plus by week 3.
5. That's always the big question. I had the nomograms and all the reports and studies, but "your mileage may vary." A recurrence could always happen, even years later.
6. My surgeon told me before the surgery that he would be able to spare 1 nerve but probably not the other. That is how it turned out. 3 months later I am down to one pad for security only--no real leakage--and partial erections. Still working on that part.
I would recommend Dr Peter Scardino's Prostate Book (the new 2010 revision). It is very helpful. There are also a number of other good books and resources out there. Good luck on your path.
Another concern - how many days after surgery, the urine through the catheter is going to be red?
Is it OK that the urine will be sometimes red and sometimes yellow?
Any other info regarding the catheter is welcome!!
Thanks !!!!0 -
CatheterPerineum said:Thank you all for your valuable information
Another concern - how many days after surgery, the urine through the catheter is going to be red?
Is it OK that the urine will be sometimes red and sometimes yellow?
Any other info regarding the catheter is welcome!!
Thanks !!!!
In my case, I had the surgery on March 1st and the catheter came out on March 9th. I had almost no blood in my urine the entire time, so it was yellow. However, it is normal to have some blood. They will give you very complete instructions about what to watch for and how to care for the catheter before they send you home. When the nurse took the catheter out it was also no big deal, or at least it wasn't for me. No pain at all and it went very easily. I also had 2 drains left in went I went home from surgery. This doesn't always happen, but can especially after a large lymph node dissection. They were more of a bother to me--probably because I hadn't heard about them before the surgery and wasn't expecting them. They're easy to take care of--just another little "pleasure" in the process. They took them out the same day as the catheter and they did hurt when they came out.
John0 -
out of topic questionSeattleJ said:Catheter
In my case, I had the surgery on March 1st and the catheter came out on March 9th. I had almost no blood in my urine the entire time, so it was yellow. However, it is normal to have some blood. They will give you very complete instructions about what to watch for and how to care for the catheter before they send you home. When the nurse took the catheter out it was also no big deal, or at least it wasn't for me. No pain at all and it went very easily. I also had 2 drains left in went I went home from surgery. This doesn't always happen, but can especially after a large lymph node dissection. They were more of a bother to me--probably because I hadn't heard about them before the surgery and wasn't expecting them. They're easy to take care of--just another little "pleasure" in the process. They took them out the same day as the catheter and they did hurt when they came out.
John
Hello again, I have some out of topic question -
How is the surgery report written?
Is it written posteriori by the surgeon (after the surgery is completed), or
is it written during the surgery (like in court) such as the surgeon tells what he is doing and someone else writes it down?
Thanks !!0 -
???Perineum said:out of topic question
Hello again, I have some out of topic question -
How is the surgery report written?
Is it written posteriori by the surgeon (after the surgery is completed), or
is it written during the surgery (like in court) such as the surgeon tells what he is doing and someone else writes it down?
Thanks !!
I have no idea but the question doesn't make much sense to me. If the surgeon is good and you feel that the treatment you selected is appropriate for you why would you care how he/she writes the report? What has that got to do with anything?
John0 -
John, "...most of the time we have to write reports"SeattleJ said:???
I have no idea but the question doesn't make much sense to me. If the surgeon is good and you feel that the treatment you selected is appropriate for you why would you care how he/she writes the report? What has that got to do with anything?
John
John
Your post made me laugh. Thanks.
Reading Perineum posts in this and other threads makes me think that he/she is not a patient of prostate cancer.
I recall when staying in the hospital for surgery, one young doctor who would come to my room every day just for chatting. He was preparing his thesis and wanted to listen about my researches that could give him ideas on prostate cancer diagnosis, treatments, etc.
His questions were so minoucious that made me return a question and said “what are they teaching you at the medical school, dancing?” to which he surprized me replying; “We learn that too but most of the time we have to write reports”.
VG0 -
Unfortunately I do a patient of PCVascodaGama said:John, "...most of the time we have to write reports"
John
Your post made me laugh. Thanks.
Reading Perineum posts in this and other threads makes me think that he/she is not a patient of prostate cancer.
I recall when staying in the hospital for surgery, one young doctor who would come to my room every day just for chatting. He was preparing his thesis and wanted to listen about my researches that could give him ideas on prostate cancer diagnosis, treatments, etc.
His questions were so minoucious that made me return a question and said “what are they teaching you at the medical school, dancing?” to which he surprized me replying; “We learn that too but most of the time we have to write reports”.
VG
The reading since my diagnose made me curious about all those medical issues, surgery...
I'm just want to know everything I can about this, like I do on every other important thing in my life..
VG, thank you very much for all the information which helped me understand my situation.
You've answered all my questions.. Unfortunately, the signet ring is really rare..
I'm considering the open surgery, and really afraid..
I've postponed it until I receive the endorectal MRI result and then decide what to do.
I really afraid of the catheter and blood in my urine... and the loss of control of my urine.
I'm also worried about what exactly my surgeon should cut and remove from my body..
Just the prostate? how many lymph nodes? nerves? And many other stuff that are not really discussed, and seems so important in order to maximally remove all the cancer out.0 -
Perineum, You are doing the right thingbdhilton said:P,
I do not see any stats of
P,
I do not see any stats of your biopsy posted here? Perhaps if you included your Gleason score and PSA folks could provide more insight for you.
Perineum
You are doing the right thing in gathering detailed information about your diagnosis treatment and outcome. However you do understand that guys here in this forum and in others have limited knowledge of the whole aspect ruling cancer care or even about matters that are required but indirect to the treatment.
I would recommend you to trust the capabilities of the team looking at your case, as well as the facilities where you will be diagnosed and treated (in Israel?). It will give you peace of mind.
The word Cancer is scaring, to have it is terrible, to treat it is problematic and to accept it is difficult but we have the power to overcome it. Think positively and you will see it as much as any other incidence that once occurred in your life. You will survive it again.
As Hilton says above we do not know details about your case. Many guys in this forum are very acknowledgeable on PCa and surely would help you in understanding the aspects of your problem, but you have to share your experiences and results.
Surgery is an excellent treatment for prostate cancer if the case is considered “contained”. That means to have the whole cancer inside the prostate gland and, once removed from our body, we become cancer free (cured). Tests to certify that the cancer is contained are not 100% accurate, but they can give an idea of what one could expect.
Failure is always possible but it is not the end of the “journey”. It is just another bump in the road.
For an overlook about a complete surgery and what is done you can listen to this video and read about it in these sites;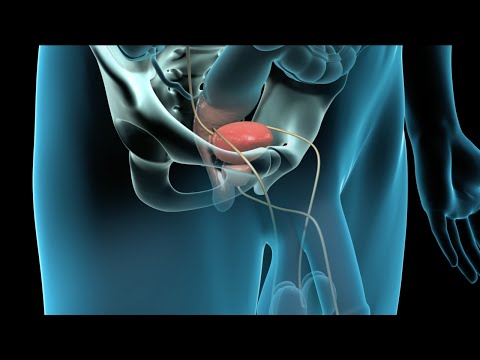 http://www.youtube.com/watch?v=rGakMycKnOs
http://www.youtube.com/watch?v=rGakMycKnOs
http://www.webmd.com/prostate-cancer/radical-prostatectomy-operation
http://www.hamiltonhealthsciences.ca/documents/Patient Education/RadicalProstateSurgery-th.pdf
http://www.webmd.com/prostate-cancer/prostate-cancer-radical-prostatectomy
Do not be so anxious but foresee the success.
VGama
Note: I want to add a word on the eMRI test, which is one of the advanced ways to check for metastasis. If this tests shows any lesion then radiation may be a better choise. However, if your doctor with the eMRI results still believes that RP is proper, try to delay the surgery and get the opinion from another surgeon. That will give you peace.
Your diagnosis is indicative of success in either treatment.0 -
My dataVascodaGama said:Perineum, You are doing the right thing
Perineum
You are doing the right thing in gathering detailed information about your diagnosis treatment and outcome. However you do understand that guys here in this forum and in others have limited knowledge of the whole aspect ruling cancer care or even about matters that are required but indirect to the treatment.
I would recommend you to trust the capabilities of the team looking at your case, as well as the facilities where you will be diagnosed and treated (in Israel?). It will give you peace of mind.
The word Cancer is scaring, to have it is terrible, to treat it is problematic and to accept it is difficult but we have the power to overcome it. Think positively and you will see it as much as any other incidence that once occurred in your life. You will survive it again.
As Hilton says above we do not know details about your case. Many guys in this forum are very acknowledgeable on PCa and surely would help you in understanding the aspects of your problem, but you have to share your experiences and results.
Surgery is an excellent treatment for prostate cancer if the case is considered “contained”. That means to have the whole cancer inside the prostate gland and, once removed from our body, we become cancer free (cured). Tests to certify that the cancer is contained are not 100% accurate, but they can give an idea of what one could expect.
Failure is always possible but it is not the end of the “journey”. It is just another bump in the road.
For an overlook about a complete surgery and what is done you can listen to this video and read about it in these sites;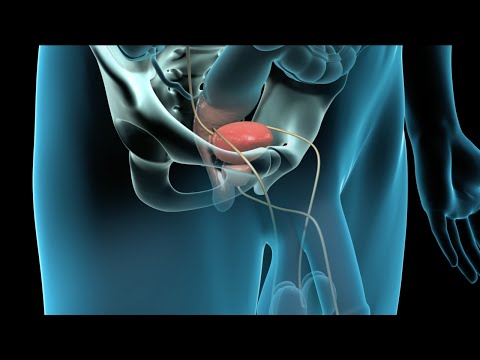 http://www.youtube.com/watch?v=rGakMycKnOs
http://www.youtube.com/watch?v=rGakMycKnOs
http://www.webmd.com/prostate-cancer/radical-prostatectomy-operation
http://www.hamiltonhealthsciences.ca/documents/Patient Education/RadicalProstateSurgery-th.pdf
http://www.webmd.com/prostate-cancer/prostate-cancer-radical-prostatectomy
Do not be so anxious but foresee the success.
VGama
Note: I want to add a word on the eMRI test, which is one of the advanced ways to check for metastasis. If this tests shows any lesion then radiation may be a better choise. However, if your doctor with the eMRI results still believes that RP is proper, try to delay the surgery and get the opinion from another surgeon. That will give you peace.
Your diagnosis is indicative of success in either treatment.
VG, Thank you very much for the information and support. I really appreciate it.
My PC details:
63 years old.
PSA elevated from 4.5 in 2004 to 9 in 2011.
Biopsy positive on 1/12 tissue cores. GS=8(4+4).
Biopsy revision was positive 1/12 tissue cores.
GS=9(5+4). Signet ring cell carcinoma (very rare).
CT, bone scan - negative
Endorectal MRI - negative (tumor not recognized in prostate nor other places like lymph nodes).
Prostate volume = 90
still considering Surgery or Radiation+Hormons.
The thing is that my oncologists deny surgery although tumor not recognized in CT, bone scan, MRI - because of the GS=9. They say that GS=8 or above should not do surgery since Radiation and Hormones will also be needed, and the surgery will not help.
I will have to make a decision very soon
What's bothering me most is the GS=9.. Oncologists say that high GS usually comes with low PSA, and it usually not seen in CT, MRI etc... so They think it already out of the prostate...
I'm thinking about surgery, but really not sure... Tough decision.0 -
I would get a second opinionPerineum said:My data
VG, Thank you very much for the information and support. I really appreciate it.
My PC details:
63 years old.
PSA elevated from 4.5 in 2004 to 9 in 2011.
Biopsy positive on 1/12 tissue cores. GS=8(4+4).
Biopsy revision was positive 1/12 tissue cores.
GS=9(5+4). Signet ring cell carcinoma (very rare).
CT, bone scan - negative
Endorectal MRI - negative (tumor not recognized in prostate nor other places like lymph nodes).
Prostate volume = 90
still considering Surgery or Radiation+Hormons.
The thing is that my oncologists deny surgery although tumor not recognized in CT, bone scan, MRI - because of the GS=9. They say that GS=8 or above should not do surgery since Radiation and Hormones will also be needed, and the surgery will not help.
I will have to make a decision very soon
What's bothering me most is the GS=9.. Oncologists say that high GS usually comes with low PSA, and it usually not seen in CT, MRI etc... so They think it already out of the prostate...
I'm thinking about surgery, but really not sure... Tough decision.
I would get a second opinion from John Hopkins or Northwestern on your biopsy. Your urologist should happily do this for you. If you are not happy with your urologist…run and run fast to another one. If you have a “little” cancer like your 1/12 is “showing in theory I would assume you are a T1c or? If so, why is surgery not an option…?
I am pretty sure everyone here who has had treatment was “on the fence” like you…It is good that you are here and asking questions as you will make the best decision for yourself. Once you make that decision (surgery, radition/hormones, nothing at all), never second guess yourself no matter what the outcome is…
I would strongly recommend diet changes (e.g. no red meat, no dairy….live like you are in the Mediterranean…)
Best to you in this journey!0 -
Perineum; I wish you peace of mindPerineum said:My data
VG, Thank you very much for the information and support. I really appreciate it.
My PC details:
63 years old.
PSA elevated from 4.5 in 2004 to 9 in 2011.
Biopsy positive on 1/12 tissue cores. GS=8(4+4).
Biopsy revision was positive 1/12 tissue cores.
GS=9(5+4). Signet ring cell carcinoma (very rare).
CT, bone scan - negative
Endorectal MRI - negative (tumor not recognized in prostate nor other places like lymph nodes).
Prostate volume = 90
still considering Surgery or Radiation+Hormons.
The thing is that my oncologists deny surgery although tumor not recognized in CT, bone scan, MRI - because of the GS=9. They say that GS=8 or above should not do surgery since Radiation and Hormones will also be needed, and the surgery will not help.
I will have to make a decision very soon
What's bothering me most is the GS=9.. Oncologists say that high GS usually comes with low PSA, and it usually not seen in CT, MRI etc... so They think it already out of the prostate...
I'm thinking about surgery, but really not sure... Tough decision.
Perineum
It is a tough decision indeed.
Gleason 9 is aggressive and if the signet-ring adenocarcinoma is present you could add another percentage on the risk.
The most concern aspect of your diagnosis is that, the cancer volume is small (1 out of 12), all tests are negative to metastasis, but the cancer may be located in the capsule of the prostate gland.
What I know about Signet-ring cancers is that they are tumours with epithelial cells whose characteristics are to infiltrate the surrounding tissue. In colon cancer they form micro tumors which are difficult to detect. It is difficult to diagnose a case similar to yours if one considers both, a high tendency for aggressivity (difficult to treat) and a high tendency for invasive of surrounded tissue.
I am not a doctor and you shouldn’t take my words in your decision. I recommend you to listen to your doctors and consult with your family.
In my opinion, Surgery is possible in all types of Gleasons, however, in your case other concerns are in play.
Surgery will require a very sharp cut to separate the gland from other organs without leaving behind any microscopic bit of the capsule. This is tricky at the bladder sphincter which sharp cut has lots to do with incontinence.
I also believe in the possibility of existing occult surrounding areas in the outer shell that cannot be seen with the tests due to the enlargement of the prostate (90).
High dosage RT may have a better choice in this case but it would probably require administration of neoadjuvant HT to shrink the prostate firstly. The radiation field close to the outer shell should receive a high dosage (isodosage) therefore to minimize damage to close organs the prostate should be smaller in size.
Surgery and radiation may work in your case but the weight is more on the side of RT.
I would recommend you to discuss the matter with your wife and obtain her opinion.
Your choice is the best and there is no look back because you really have done your homework with so many researches and consultations. No one could do it better as you did.
I wish you peace of mind.
Good luck in the treatment.
VGama0
Discussion Boards
- All Discussion Boards
- 6 CSN Information
- 6 Welcome to CSN
- 121.9K Cancer specific
- 2.8K Anal Cancer
- 446 Bladder Cancer
- 309 Bone Cancers
- 1.6K Brain Cancer
- 28.5K Breast Cancer
- 398 Childhood Cancers
- 27.9K Colorectal Cancer
- 4.6K Esophageal Cancer
- 1.2K Gynecological Cancers (other than ovarian and uterine)
- 13K Head and Neck Cancer
- 6.4K Kidney Cancer
- 672 Leukemia
- 794 Liver Cancer
- 4.1K Lung Cancer
- 5.1K Lymphoma (Hodgkin and Non-Hodgkin)
- 238 Multiple Myeloma
- 7.2K Ovarian Cancer
- 63 Pancreatic Cancer
- 487 Peritoneal Cancer
- 5.5K Prostate Cancer
- 1.2K Rare and Other Cancers
- 540 Sarcoma
- 734 Skin Cancer
- 654 Stomach Cancer
- 192 Testicular Cancer
- 1.5K Thyroid Cancer
- 5.9K Uterine/Endometrial Cancer
- 6.3K Lifestyle Discussion Boards
