The Cancer Survivors Network (CSN) is a peer support community for cancer patients, survivors, caregivers, families, and friends! CSN is a safe place to connect with others who share your interests and experiences.
Rituximab alone...? Chemo-free thoughts invited.
Comments
-
Duckhead - I believe that the poor prognosis after transformation is due to the fact the patients have multiple types of lymphoma at the same time. DLBCL does not replace the FNHL but is in addition to it. Who knows how they interact? Also it seems that the FNHL becomes more resistant to treatment with each relapse or transformation. There is a regular here whose FNHL transformed before it was even diagnosed. She was cured. Perhaps she will chime in.
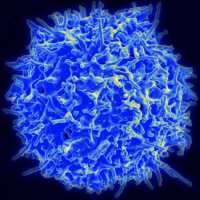
Remember - my lymphoma is not a foreign invader. It is produced in and is part of my body. The body learns to produce lymphocytes outside the bone marrow via self cloning of limitless numbers of identical lymphocytes . These cloned cells do not die as do bone marrow produced lymphocytes and thus become overpopulated and form tumors. That is lymphoma in a nutshell in my simplistic view of it. I am not a doctor.
-
CA,
I've never heard of NLPHL that did not have an abundance of CD20, but I also have never read that such an occurrence is impossible. NLPHL traditionally had so little research behind it that, even as a very aberrant HL, it was by default simply treated as classic HL, which meant ABVD. Gradually, the oncology community realized, hey, since there is CD20 here, as in NHLs, we should include Rituxan with the ABVD. Still today, some oncologist simply do not choose to add Rituxan to NLPHL patients. After my second R-ABVD infusion in 2009, I was hospitalized for three days due to neutropenia. One of the oncs on rotation came in one night and asked what disease I had, and what I was taking. I told her R-ABVD, and she said, 'Good grief ! Doesn't your doc know that HL patients don't get Rituxan ?' She was not a hematology specialist, and the point is simply that NLPHL is so rare and peculiar that even some oncologists are unfamiliar with how different it is. Many patients here over the years have shared that they were not getting Rituxan for NLPHL, despite presenting CD20.
Regarding what morphs into what, I have always read that whatever strain of lymphoma a person has, if it relapses, it will very likely either come back as what it was before, or a step or two more aggressive. Hence, Follicular would usually come back as Follicular, or Large-B NHL. Or, if not a more aggressive lymphoma, then as some form of leukemia.
-
Max,
I too used to think that CD20 expression was a must for a pathologist to conclude that it was NLPHL. Our onc was talking about potential for transformation of NLPHL to DLBCL or THRLBCL and shared that relapse with CD20 negativity was possible as well. Here is a recent paper on this:
All the best.
-
I thought about starting a new topic but with so many great contributors in this thread, I decided to continue off topic here instead.
My end of treatment PET scan report was uploaded to the patients’ portal yesterday. I am not entirely sure what to make of it and scouring the internet hasn’t helped a great deal. The appointment with my hematologist/oncologist is not until next week. Meanwhile, for my own education and for dialing down my curiosity (& anxiety), I thought it wouldn’t hurt to post here.
Here are the highlights.
Oncologic findings:
Index lesions - “left periaortic node measuring up to 1.7x1.5 cm SUV max 2.2 down from 6.3x4.3 cm SUV 10.4 previously…mesenteric node approximately 1.2x2.0 cm SUV 2.2 compared to 11x10 cm SUV 13.2 previously.”
lymph nodes - “majority of previously noted bulky and extensive hypermetabolic lymphadenopathy is nearly completely resolved…a few scattered minimally prominent retroperitoneal and mesenteric nodes with avidity below blood pool remain…no new or enlarging sites of disease, no sites of disease with activity above blood pool…no metastases in lungs, bones or other.”
Non-oncologic findings:
“Bilateral symmetric and diffuse adrenal gland uptake, greater than liver blood pool, which is favored reactive. Attention on follow up” (same comment also repeated under “impression”).
Impression:
”In comparison to prior PET, marked decrease in bulky extensive lymphadenopathy. While the majority of the lymphadenopathy appears resolved, there are residual minimally prominent retroperitoneal and mesenteric nodes with activity below blood pool. Deauville 2.”
While the Deauville score of 2 is a positive development and a big improvement (it was a 5 pre-treatment), I am not sure what to make of the index lesions, albeit much reduced in size along with their associated SUV, the remaining few scattered minimally prominent retroperitoneal & mesenteric nodes, albeit with avidity below blood pool, and the bilateral symmetric & diffuse adrenal gland uptake greater than liver baseline/blood pool.
I see that Deauville 1 or 2 is considered PET negative and generally accepted as a complete metabolic response (CMR) which is defined as a return of FDG uptake in previously documented lesions to a level equivalent to, or less than, residual radioactivity in normal tissues. Or is that so in my case given the findings listed? Is CMR the same thing as complete remission (CR)?
At least for me, I have a difficult time deciphering what the PET report is really saying in a big picture sense so I thought I would pick your collective brain here. Not asking you to play doctors but I am sure your comments will certainly help me ask some important questions during the upcoming visit with my doctor as to the next step forward. I welcome any inputs you may have and thank you in advance.
-
I am not a doc and only know what I have read online about these scans. It would appear that there is improvement in what was visualized and what that means, I think your doc will have to tell you.
My last PET scan was end of treatment in January and the synopsis was partially this:
COMPARISON: Prior PET/CT examinations dated 10/15/2021 and 06/24/2021. FINDINGS: NECK: There is a physiologic distribution of tracer uptake. There is no hypermetabolic lymphadenopathy in the neck. CHEST: There is no suspicious hypermetabolic lymphadenopathy. A subcentimeter left axillary lymph node with minimally increased tracer uptake on image 91 is favored to be reactive. There is no hypermetabolic pulmonary nodule. ABDOMEN AND PELVIS: There is a physiologic distribution of tracer uptake. There is no hypermetabolic lymphadenopathy. There is no hypermetabolic adrenal nodule. The spleen is normal in size and FDG avidity. There is physiologic excretion of tracer in the bowel. MUSCULOSKELETAL: Background tracer uptake in the bone marrow is within normal limits. etc. etc. etc.
IMPRESSION: 1. Complete metabolic response to treatment (Lugano/Deauville score = 1). There is no suspicious hypermetabolic lymphadenopathy above or below the diaphragm. 2. No lymphomatous involvement of the spleen or bone marrow.
My oncologist was quite happy with this and agreed to continue treatment with Rituxan maintenance for two years every other month which I am now doing. The goal is to keep the remission going. You may want to consult with your doc regarding this.
Best thoughts for you.......
-
It seems to be saying tht you are definitely headed in the right direction and have made substantial gains. The size of nodes is one thing, but the SUV is crucial. The lower the better. The percentage of decrease in SUV and the lower absolute number seem to indicate that it is on the run and while, not completely eradicated, is on the way out. Now is the time to stay the course, I am guessing, with close attention paid to future scans to monitor its behavior.
However, if it should rebound slightly, not to worry as there are other drugs and combinations to use, as well as new drugs and even clinical trials.
-
Newold & po18, thanks for your feedback.
I had a visit with my doc yesterday to discuss the PET results. He used the term “complete remission” in spite of very “slight uptake” ( his words). Surely, I have come a long way in 6 months from heavy tumor burden, pleural effusion, pulmonary embolism after my first chemo and a Deauville 5 to this.
Naturally, we had a discussion about maintenance. While it’s not my treating physician’s practice to prescribe a maintenance regimen as he believes the risk of infection outweighs the benefits just to name one (esp taking into consideration my job - more on that below), and perhaps in my case after having done Bendamustine + Rituxan (BR), he said he is not opposed to prescribing it for me if I insist on having it. In that case, it’ll be a Rituxan infusion once every two months.
I have also read some studies, esp the BRIGHT studies on maintenance following BR treatment, which state in part that a maintenance regimen does not seem beneficial in prolonging remission for those people who achieved complete remission from PET whereas there are benefits (in prolonging remission) for those who achieved partial remission.
I am seriously weighing the risk-benefit as my state of health now may allow me to return to work as an airline pilot and finish out the last 3 years of my career before mandatory retirement kicks in. So the risk of catching something is certainly there if I stay constantly immunodeficient going forward while I return to work. I have read a few posts here from people who had to stop maintenance due to infections and complications. I suppose one has to be vigilant about hygiene and living habits. Being on an airplane regularly certainly won’t help in that endeavor.
-
Hi Duckhead - very glad you have achieved the CR status and best wishes on keeping it that way. I just suspended Rituxan maintenance treatments after developing a pneumonitis infection after my last treatment in Jan (I finished BR frontline for my FL in July 2021 and started 1 every 3 months of Rituxan in October 2021). My hematologist/oncologist has voiced similar concerns as your doc - that the risks of infection (and other side effects) may outweigh the benefits of the treatment. Her reasoning in my case has been 1) I achieved CR after 3 months of BR treatment (the post-6 months PET had same results as at 3 months), so after achieving CR I had 5 more Rituxan treatments as of the Jan treatment already (the 3 BR plus 2 maintenance), and 2) this is my second cancer - I lost a lung to neuro-endocrine cancer in the mid-90s and live with elevated risk of lung infection in any case. She has reminded me what we currently know about maintenance therapy based on available evidence - that it can prolong the time to another lymphoma event, but generally does not prolong life. I am currently facing the decision of either staying off treatment, or resuming it on my July cycle. Again my doc favors discontinuing given my CR, general state of good health, and other risk factors. There is no right answer, it must fit you and your circumstances. Personally I found trying to get back to normal lifestyle, resume pre-treatment work burdens, and avoid infection risk all very challenging while getting injected with R-Mab every three months - it did knock me out for a few days each treatment cycle, and it really hit my white blood counts sharply for that entire 3 months and forced me to alter the lifestyle to avoid infection risks. Need to weigh the quality of life, life priorities, and potential health benefits vs risks on this one - maintenance very 2 months may not be necessary to desirable for all of us. Good luck and best wishes!
-
I'm glad your doc gave you a good read on your PET. Maintenance seems to be a very controversial topic with many of these docs. I did a lot or reading and research and discussing prior to undertaking this course. There were those studies that I read that clearly stated that there may very well have been an OS improvement, but the studies did not go on long enough to illustrate that. One study that I read that was done by a Veterans Hospital clearly stated that docs should not tell patients that there is no OS benefit for this reason. In any case, I just finished my 3rd infusion, side effects are minimal and as we are retired can avoid interacting in situations that may threaten my immune system. I am 74 and if I can avoid further treatment for progression that would be fine with me. In any case if something becomes problematic, I can always discontinue. Scheduled for a CT scan in a couple of months prior to my next treatment to see if things have remained in remission from the last PET in January.
Best to you all.
-
My first treatment for FNHL stage 4 was R. Back then you had the choice of 4 or 10 weekly treatments to start. I went for ten. My second opinion at MD Anderson 4 months after beginning therapy verified NED. However MDA suggested I continue with R therapy once every 8 weeks for two years. I was clearly told in no uncertain terms that the maintenance could offer longer periods between relapses but showed no evidence of improvement in OS. It was incurable and I would die with it or from it. At the end of maintenance I had experienced zero infections. I went thru relapse 4 1/2 years later and had chemo. We started R maintenance but ended it when I developed a severe sinus infection. My cancer can be seen on scans but does not appear active so I am on watch and wait. I think R maintenance was a big quality of life enhancement for me and I would do it again. I had some really good years. I fully expect my FNHL will require treatment again. Hopefully I am wrong about that.
-
I had six treatments of R-Bendeka or Treanda which is the same thing (bendumastine) without much problem, OTHER than Afib from caffeine, so watch the coffee, chocolate, cola and fatigue which I still have. This did not appear to be from the Rituxan as this has not been a problem with Rituxan maintenance. This entire process is fear and anxiety producing on its own without drugs, but it could certainly be a side effect. I suppose it could also be caused by the steroids they give you to counter side effects.
-
I just completed 6 treatments of bendamustine-Rituximab (B-R) following a grade 1-2, stage IV follicular lymphoma with a heavy tumor burden diagnosis. PET scan from three weeks ago showed a complete metabolic response.
I had a severe reaction during the first infusion of Rituximab when it was increased to the rate of 100 mg/hr. I developed extreme chills and uncontrollable convulsions. I was then injected with some kind of steroid and also a heavy dose of Benadryl. I was out and ended up staying in the hospital overnight while they dialed down the Rituximab infusion rate back to 50 mg/hr. It took almost the entire night to complete the 800 mg-bag of Rituximab.
A week later while at home, I developed a 103 F fever. Checked into ER and long story short, I ended up being hospitalized for 6 days. During my hospital stay, a CT scan revealed blood clots in my lungs ( pulmonary embolism or PE). I had moderate chest pain and some light coughing. My hematologist said it was likely provoked by the chemo immunotherapy treatment. I was put on blood thinner for 6 months. In fact, I just got off the meds. After a month or so on the blood thinner, I felt normal again with no chest pain or coughing.
No severe reactions to the second cycle of B-R therapy ( even at maximum infusion rate) other than persistent abdominal pain for a couple of weeks due to constipation. In retrospect, it’s best to stay ahead of it. Cycles 3-6, I had hardly any adverse reaction whatsoever other than itching of the skin ( mostly in the torso). The itching ( I would call it light in intensity) was persistent throughout treatment and only went away a few weeks ago, about 1 month after the completion of B-R.
I thought I should also mention this observation here. While it is not a normal protocol to do a pulmonary function test (PFT) following completion of chemo, I had to do one to fulfill the return-to-work requirement due to my PE. The results took me completely by surprise because I have been feeling great, been walking quite a bit and even started jogging again. I was normal in the spirometry portion of the PFT but in the diffuse lung capacity test, I registered below normal range and a mildly decreased diffusion in lung capacity.
Maybe my PE has not been completely resolved even though I have had no symptoms. Or perhaps the chemo immunotherapy regimen caused some inflammation in my lungs, which is what I am hoping, rather than the possibility that there has been some permanent scarring or damage to my lungs.
After seeing my PFT results, I looked into Rituximab some more, specifically as it relates to the lungs, and came across this excerpt below from Mayo. Somebody on this site also mentioned this potential problem on a different thread. I don’t know what to think but I have an appointment with a pulmonologist later this week. Not sure anything can be done about it if it’s part of your treatment plan other than to know that all drugs have side effects, some potentially more serious than others. Anyway, thought I’d mention it here.
Best of luck in your treatment.
Many drugs can damage your lungs, especially:
- Chemotherapy drugs. Drugs designed to kill cancer cells, such as methotrexate (Otrexup, Trexall, others) and cyclophosphamide, can also damage lung tissue.
- Heart medications. Some drugs used to treat irregular heartbeats, such as amiodarone (Nexterone, Pacerone) or propranolol (Inderal, Innopran), may harm lung tissue.
- Some antibiotics. Nitrofurantoin (Macrobid, Macrodantin, others) and ethambutol (Myambutol) can cause lung damage.
- Anti-inflammatory drugs. Certain anti-inflammatory drugs, such as rituximab (Rituxan) or sulfasalazine (Azulfidine), can cause lung damage.
-
Duckhead, I also had six treatments of R-B and just had my 3rd maintenance dose of R. Since I started all this a year ago, I noticed a degree of SOB, cutting the lawn with a push mower, walking up a hill, etc. The oncologist said that my blood work was not the cause and my PETS have shown nothing that would do it. I still walk 40 miles a week and ride my bike a little. It is noticeable riding a bike more so than walking but tends to improve as you warm up a bit and push things. I have added some hills to this regimen and that has probably improved things somewhat. I would not be surprised as you note that Rituxan has something to do with this. However, it is still my intent to finish two years of maintenance therapy if it continues to go well.
-
Thanks newoldguy, good information. Very interesting on the AFIB. I am now dealing with rapid heart rates upon movement and palpitations/heartbeat pauses. Assume it’s inflammation causes by the cancer and chemo regiment. I know my Hematologist has a plan to dial in my dosing for my next cycle- bit more steroids up front. But again stills a bit unnerving. Appreciate your input!
Discussion Boards
- All Discussion Boards
- 6 Cancer Survivors Network Information
- 6 Welcome to CSN
- 122.6K Cancer specific
- 2.8K Anal Cancer
- 457 Bladder Cancer
- 312 Bone Cancers
- 1.7K Brain Cancer
- 28.6K Breast Cancer
- 407 Childhood Cancers
- 28K Colorectal Cancer
- 4.6K Esophageal Cancer
- 1.2K Gynecological Cancers (other than ovarian and uterine)
- 13.1K Head and Neck Cancer
- 6.4K Kidney Cancer
- 684 Leukemia
- 804 Liver Cancer
- 4.2K Lung Cancer
- 5.1K Lymphoma (Hodgkin and Non-Hodgkin)
- 242 Multiple Myeloma
- 7.2K Ovarian Cancer
- 70 Pancreatic Cancer
- 493 Peritoneal Cancer
- 5.7K Prostate Cancer
- 1.2K Rare and Other Cancers
- 544 Sarcoma
- 744 Skin Cancer
- 661 Stomach Cancer
- 193 Testicular Cancer
- 1.5K Thyroid Cancer
- 5.9K Uterine/Endometrial Cancer
- 6.4K Lifestyle Discussion Boards