The Cancer Survivors Network (CSN) is a peer support community for cancer patients, survivors, caregivers, families, and friends! CSN is a safe place to connect with others who share your interests and experiences.
Got diagnosed 2 weeks ago. Age 30, otherwise perfect health
Oh man.
Was having heartburn for ~3 months before doing an endoscopy. They found a mass, stage III esophogial cancer, not spread to any organs, but in probably 5-7 lymph nodes. Starting chemo+radiation next week, followed by surgery. Surgery is the goal, although 1-2 lymph nodes seem to be in dangeorus spots.
Needless to say, this is devastating to my family and myself. I'm not a drinker, never smoked, been athlete all my life. Otherwise perfect health. 4 days ago, bloodwork came in perfect.
Hope is that my age, strength, and overall good health will be big factors in my treatment.
At the moment, I am terrified. I can't leave my 28yo wife behind, I can't have my parents have to see me go through this. I can't browse this forum since one negative thing throws me into desparation. Only thing I was able to do is post this thread.
Comments
-
mister_eko~U need 2 come back if U want 2 talk 2 EC survivors!
Dear mister_eko
How about if you heard from an Esophageal Cancer patient, diagnosed back in 2002, and received the very least invasive Esophagectomy, known as the Ivor Lewis Minimally Invasive Esophagectomy. “mister” you are indeed “blessed” to be diagnosed at a stage which falls within the “operable” stage. Others here would love to be in your place, believe me.
My husband didn’t drink, smoke, (or even run around with women
 ) he only had a hiccup. He didn’t even have heartburn! You are not alone, and you can be a survivor as are many here.
) he only had a hiccup. He didn’t even have heartburn! You are not alone, and you can be a survivor as are many here.So don’t linger long in your “frightened” state. You need to be a quick learner. So if you want to learn more about Esophageal Cancer patients who have been “through it all” and are survivors check back in. “mister_eko you need to get smart” real quickly, so you can make the very best decisions. This is as informative a link as you will find. Anything we say here should be checked out with your doctor. “I dare you to read more here!” We who have been through this cancer and come out on the other side aren’t here for “our health”, we’re here for “newbies” like you. So I’m glad you came on one time, and I hope you will soon get your emotions under control. You can’t make decisions based on “emotions”, you’ve got to make decisions based on “facts”.
So if you want to talk to my husband, or others here, and learn more about his successful surgery, and is celebrating his 14th year of Survival with “no evidence of disease”, send me a message, or write more here.
Good grief, life isn’t all roses, and you’re big enough and old enough to face this and take control of this diagnosis. There are many Stage IV EC patients here who would love to trade places with you. After all, none of us “ordered” this, and at one time they were healthy too. Nobody would get in line to have this cancer on an “elective” basis, but we all would like to come in under the “Stage 3” wire! if we have to be a member of this group!
Most sincerely,
Loretta Marshall (Wife of William) William diagnosed with Adenocarcinoma at the Gastroesophageal junction (T3N1M0). Successful laparoscopic Ivor Lewis Esophagectomy performed by Dr. James D. Luketich at the University of Pittsburgh Medical Center on May 17, 2003!
P.S. We could be of more help if you would tell us more than your age. We know you're frightened, but no more so than any of the rest of us when we were told "you have cancer!" So can you fill us in as to who your doctors are, what medical facility you've been treated and with what, what have the doctors said as far as a treatment protocol, and have you had a second opinion? What kind of tests have you had to date?
You will be much less frightened the more you know, believe me. Armed with the most knowledge will get you the very best treatments. But we can't help if you don't want to talk to us. Surely you've not lived 30 years and never had a disappointment in life prior to this.
-
hi there, thanks for a nice post. I realize that I have it way better than a lot of people here, but it's still a Shock.
I've been diagnosed with endoscopy at Emory Hospital in Atlanta Georgia. I also work there. Mass is about 3cm big, doesn't seem to have penetrated walls, and is contained within lymph nodes. Pet scan showed 5-7 of them infected, one or two being around lungs and aorta and my surgeon, dr. Seth Force, very well known for this kind of surgery, isn't confident he could reach these lymph nodes.
I have 5.5 weeks of chemo and radiation Ahead. Chemo on Mondays and radiation Monday through Friday. Then aftee 5 weeks, another pet scan to see if surgery can help. That wait will be the worst part.
I did did have second opinion at Piedmont hospital which confirmed all that Emory said. So far I only had a pet scan done, and bloodwork which came back perfect.
-
-
...agree with Loretta
Hi Mister eko....I'm pat. My 'handle' is ECLC which stands for Esophageal Cancer/Lung Cancer. I was just diagnosed with esophageal cancer 3 weeks ago and am waiting to hear back from Hopkins to get a surgery date.
It's my lung cancer I want to talk to you about first though. I was training for a marathon, in very good shape and 34 years old. I had my beautiful wife (managed to keep her), an 11 year old son and 7 year old daughter. Out of nowhere I was diagnosed with lung cancer. Thankfully, my age and my health had a lot to do with how well I made it through the treatment so while you think your life sucks, it would definitely suck more if you weren't in shape. To tell you that we're not terrified would be a lie but you've got to be able to face the enemy head on. You're going start using words you've never heard of before...'resection', 'aspiration', 'anastomosis', etc. You need to research treatments on your own too. I sent my surgeon two medical abstracts this week on various treatment regimens that I'm interested in discussing. If you don't take charge of yourself, you stand a better chance of dying...simply put. You need to be comfortable with your oncologist too...one thing that I always tell people is that if you die, your oncologist will have another patient...your 28 year old wife will NOT have another you....so this is important stuff.
You will find that the people on this web site are a family of sorts. A lot of us have 'been there'. We've made mistakes along the way and have learned from those mistakes...we're happy to share our experiences with you so that you don't make those same mistakes especially since we're all running against the clock. The longer we take or the more mistakes we make the more this damn thing inside us grows.
Rather than get in to my story about lung cancer and esophageal cancer, I'll leave this post as it stands. I am more than happy to answer any questions you may have and will share all of my 'adventures' with you too.
Look forward to hearing from you....pat
-
mister_eko - My pleasure to share lots of good info w/U tomorrowmister_eko said:What stage was your husband
What stage was your husband when diagnosed? can you tell me more about his process?
Yes, I will gladly tell you more about my husband's diagnosis and his process. But you might want to take a day off from work to read it all. My husband's stage was "Adenocarcinoma at the GE junction" (Stage III - T3N1M0). So look for a long answer tomorrow. He is a poster child for EC. He had pre-op (neo-adjuvant) chemo of Carboplatin & 5-FU plus 25 radiation treatments - then a totally laparoscopic procedure with small band-aid cuts instead of massive incisions. He was in and out of the hospital in 5 days, and downtown shopping with me in Pittsburgh on Day 8. But that's an "in-a-nut-shell" synopsis. Obviously the "nut shell" is a large one! But there is life after Esophageal Cancer.
Briefly, I would only go to a major cancer hospital where Minimally Invasive Esophagectomies is one of their top specialties. Esophageal Cancer is classified as a "challenging diagnosis" and all hospitals rank differently when it comes to treating this particular cancer. So even though you work at Emory, there may be other hospitals that rank higher in the treatment of Esophageal Cancer. So don't be afraid to seek the "top doctors" because your aim is taking care of NO. 1 and that's YOU. So I hope you're a quick learner.
Loretta
Also every EC patient should be tested to see if they are HER2 positive. Some patients have an "oncogene" which is "over expressive" and thus the cancer spreads more quickly. HERCEPTIN is not a chemo drug, but is given in addition to chemo drugs.
But I can't begin to tell you tonight, all that I wish to convey. But thanks for replying. Will definitely fill you in on things you NEED to know to be confident that you are getting the very best treatment possible.
Loretta
-
Hello
Hello mr_eko,
It's an insane shock to get such a diagnosis at such a young age, but your youth & strength are enormous assets in your fight. I was 40 my 1st time around (stage III, also) and I know how it feels to get a disease that you think is largely for old people. EC, though, tends to strike younger than most other cancers. As much as youth & physical strength are assets, so are attitude and mental strength. With radiation, chemo and surgery upcoming, you are going to be put through the wringer. As rough as the radiation and surgery can be, you are fortunate to be a candidate for both--when it has metastasized, radiation and surgery frequently aren't options for treatment. A determination to get through it all for your wife will go a long way towards making it successfully.
My 1st time around, I had chemo/radiation, then surgery, then a bonus course of chemo, so I have an idea what you're headed for. It was pretty rough and I was with top of the line folks. Please make sure that you're dealing with people who deal with EC for a living. I'm not familiar with the hospitals you've mentioned, but I hope they're high quality centers.
I'd like to echo what Loretta and Pat have said--It is of enormous importance for you & your family to become educated and take responsibility for your treatment. If they let something falls through the cracks, it's a learning experience for them, but it's potentially deadly for you. You have the most to gain/lose, so you need to be front & center as a member of your treatment team.
Hoping the best for you,
Ed
-
So sorry you find yourself here
Mister_eko,
I am so sorry you find yourself here. The good news is you are young and strong. That is important when dealing with chemotherapy and surgery. Having a young immune system is valuable as well. I was 61 when I was diagnosed. I had surgery and chemotherapy and almost seven years later I am still here and getting clear scans so far.
I can only echo the comments of the folks who have posted above. I would encourage you to investigate a second opinion at a cancer center that has a national reputation for dealing with esophageal cancer. Since you mentioned Emory I assume you are in the Atlanta area. You are not that far from MD Anderson or Duke Cancer Center. Both have excellent reputations for dealing with esophageal cancer.
I know you are very frightened right now, but just take things one day at a time.
Wishing you the best as you complete your treatment and recovery.
Best Regards,
Paul Adams
McCormick, South Carolina
DX 10/2009 T2N1M0 Stage IIB - Ivor Lewis Surgery 12/3/2009
Post Surgery Chemotherapy 2/2009 – 6/2009 Cisplatin, Epirubicin, 5 FU
Six Year Survivor -
guys, thank you all so much
guys, thank you all so much for chiming in. I do feel much better. Where would you suggest I go looking for other treatment options? So far, I know about HER2 and Immuno Oncology, but doctors told me both would be options should chemo, radiation and surgery don't kill it completely
I got a second opinion form Piedmont Hospital which is a part of Md Anderson group and they agreed with Emory. Emory also has the best surgeon for this type of cancer, dr. SeTh Force.
-
Ed, was the second round ofDeathorglory said:Hello
Hello mr_eko,
It's an insane shock to get such a diagnosis at such a young age, but your youth & strength are enormous assets in your fight. I was 40 my 1st time around (stage III, also) and I know how it feels to get a disease that you think is largely for old people. EC, though, tends to strike younger than most other cancers. As much as youth & physical strength are assets, so are attitude and mental strength. With radiation, chemo and surgery upcoming, you are going to be put through the wringer. As rough as the radiation and surgery can be, you are fortunate to be a candidate for both--when it has metastasized, radiation and surgery frequently aren't options for treatment. A determination to get through it all for your wife will go a long way towards making it successfully.
My 1st time around, I had chemo/radiation, then surgery, then a bonus course of chemo, so I have an idea what you're headed for. It was pretty rough and I was with top of the line folks. Please make sure that you're dealing with people who deal with EC for a living. I'm not familiar with the hospitals you've mentioned, but I hope they're high quality centers.
I'd like to echo what Loretta and Pat have said--It is of enormous importance for you & your family to become educated and take responsibility for your treatment. If they let something falls through the cracks, it's a learning experience for them, but it's potentially deadly for you. You have the most to gain/lose, so you need to be front & center as a member of your treatment team.
Hoping the best for you,
Ed
Ed, was the second round of chemo after survey necessary because they couldn't get some parts in surgery?
-
Bonus Chemomister_eko said:Ed, was the second round of
Ed, was the second round of chemo after survey necessary because they couldn't get some parts in surgery?
No, the course of treatment for me was to have radiation with chemo first. The radiation was the primary treatment, the chemo was in a lighter dose designed to "activate" the radiation and make it more effective. Then surgery, b/c there is no way to know if the chemo/radiation killed everything until pathology is performed on the removed esophagus. Then came the 2nd round of chemo, which was full strength (much stronger than the 1st time) to make triple sure that all of the cancer was killed. The 2nd round of chemo was basically bayonetting the corpses on the battlefield to make sure there were no survivors.
Each part of the treatment plan was a success. The surgery revealed that the radiation had left no cancer. Obviously the surgery removed anywhere remaining cancer was hiding and the bonus chemo cleaned up anything else. It was a very aggressive course of treatment b/c I was young and we weren't hoping to buy me a couple of years, but a few decades. Turns out the cancer came back a few years later anyway, but I'd still take the most aggressive option available again if I had it to do over.
Hope your treatment starts smoothly this week,
Ed
-
Ed, thanks for the reply.Deathorglory said:Bonus Chemo
No, the course of treatment for me was to have radiation with chemo first. The radiation was the primary treatment, the chemo was in a lighter dose designed to "activate" the radiation and make it more effective. Then surgery, b/c there is no way to know if the chemo/radiation killed everything until pathology is performed on the removed esophagus. Then came the 2nd round of chemo, which was full strength (much stronger than the 1st time) to make triple sure that all of the cancer was killed. The 2nd round of chemo was basically bayonetting the corpses on the battlefield to make sure there were no survivors.
Each part of the treatment plan was a success. The surgery revealed that the radiation had left no cancer. Obviously the surgery removed anywhere remaining cancer was hiding and the bonus chemo cleaned up anything else. It was a very aggressive course of treatment b/c I was young and we weren't hoping to buy me a couple of years, but a few decades. Turns out the cancer came back a few years later anyway, but I'd still take the most aggressive option available again if I had it to do over.
Hope your treatment starts smoothly this week,
Ed
Ed, thanks for the reply. They're going with aggressive treatment with me as well, but no second round of chemo was mentioned. I'll ask them about it. Did they ever mention HER2 cells to you?
how much later did the cancer return? And was it related?
-
mister_eko said:
Ed, thanks for the reply.
Ed, thanks for the reply. They're going with aggressive treatment with me as well, but no second round of chemo was mentioned. I'll ask them about it. Did they ever mention HER2 cells to you?
how much later did the cancer return? And was it related?
The cancer came back about 3 years after I was done treatment. It was a recurrence of the EC, not a different cancer. It was in my lung, which means it had metastized and I was stage IV at that point. Fortunately herceptin had just been approved for metastatic EC in folks who test postive for HER overexpression.
Since I was stage IV, radiation and surgery weren't options for me and I was given a particularly grim prognosis. I could only do chemo, which wasn't as aggressive as I wanted to be, so I went and got another opinion from a world class cancer center. They told me that my oncologist was correct and that my best bet was to stay with her and do the chemo she recommended. Since I was HER2+, herceptin was prescribed to accompany the chemo. I'm still testing clean almost five years since I was diagnosed with the recurrence. I have been very fortunate in that I responded extremely well to the chemo and herceptin.
-
"mister_eko"-FYI-CHEMOTHERAPY TIPS that worked well 4 memister_eko said:guys, thank you all so much
guys, thank you all so much for chiming in. I do feel much better. Where would you suggest I go looking for other treatment options? So far, I know about HER2 and Immuno Oncology, but doctors told me both would be options should chemo, radiation and surgery don't kill it completely
I got a second opinion form Piedmont Hospital which is a part of Md Anderson group and they agreed with Emory. Emory also has the best surgeon for this type of cancer, dr. SeTh Force.
Hello again “mister”
Since you’re starting chemo and radiation this week, thought you would like to hear how I responded to mine. I have had two different regimens of chemotherapy, one 6-regimen treatment, each 3 weeks apart, in 2013 and another in 2015. The way people respond to chemo will vary from one person to another, even when the chemo cocktail is the same. You may “sail through with few side effects or as you progress, the treatments may take a toll on you physically. Either result will be normal, keeping in mind that chemo is never a “piece of cake”, but it is tolerable and oft times very effective.
When my husband William went through his pre-op chemo treatments of Carboplatin and 5-FU, he fared much better than did I when I had my chemo treatments of Carboplatin and Taxol. My first treatment was so awful, I truly almost died. It wasn’t 2 minutes into my treatment that my whole spine went into a jerking motion similar to that of a “jack hammer”. I felt dizzy, faint and almost passed out. My husband said I turned “red” all over. The nurses immediately yanked out the tube that went into my medi-port and began giving me something to counteract my awful reaction. Afterwards I said to the nurse, I thought I was going to die. To which she responded, “I will tell you that we have coded some patients.” My first visit lasted from about 8:15 A.M. until 7:00 PM that night, and it is one I shall never forget.
The first place you will visit will be the lab. There you will have a Complete Blood Count (CBC). This will occur each time you have a chemo treatment. For instance if your white blood count (immune cells) are too low, a chemo session will not take place. But I never had that to happen because my doctor called me back the day following my chemo treatments, and gave me a HYDRATION treatment, plus some steroids, and an injection of NEULASTA. NEULASTA will quickly replenish the White Blood Count (WBC) (infection fighting cells.)
My treatments consisted of 6 separate sessions three weeks apart. I had a CT scan after the first 3 treatments to see how effective they were. If there is no change in the eradication of tumors, the oncologist may wish to change the chemo agent to that of a different one.
Then I had another CT scan upon completion. My first treatments began in early February of 2013. The tumors were reduced in number and size at that time enough to qualify for Cytoreductive surgery (CRS). I had surgery July 1, 2013. I don’t always find it necessary to talk about my own cancer on the EC site, but this is my own personal experience with chemo. As I said others will differ.
As for my husband, he had radiation as well, I did not. He drove himself to the radiology clinic, and all in all, he had an easy time of chemo. So that is always our desire. However, it can be “wicked” with many unpleasant side effects. And at 30, you have a nice head of hair no doubt. However, depending on the type of chemo you will receive, the hair may fall out. If that begins to happen you may as well shave your head. Not to worry, it will return, but hopefully the cancer won’t.
When my husband’s treatments were completed, PET scan showed “NO CANCER”. However, we were told ahead of time, even if that happens, the Esophagectomy is part of the process. That is because sometimes residual cancer is not picked up on the scan, but will be detected during the surgery. Moreover, if after the surgery, there is any remaining cancer cells, post-op (adjuvant) chemo will be given. However, my husband’s surgeon, Dr. James D. Luketich, does not like to order more radiation after surgery. Radiation can damage the heart, and does cause a great deal of scar tissue as well. But thankfully, out of the 22 lymph nodes tested for residual cancer, none were found to be infected, so no more treatment was necessary.
My second session of chemo treatments began June 11, 2015 and ended September 2015. I am now in a “holding pattern”. Even now my CA-125 (tumor marker for Ovarian Cancer) is rising considerably, I’m not going to rush to “try” something else until a more debilitating physical condition arises. And “when it happens, it happens”. I’m not going to spend my days living weeks ahead fretting over things over which I have no control. I want to live while I’m living, and not spend my days wallowing in a worry pit. I have developed that attitude from observing some dear ones that spend their days worrying about things that “might” happen. This kind of attitude will keep you from enjoying the day you have before you. And so, I hope that is the attitude that you and will take.
With that in mind, I will tell you that chemotherapy treatments are cumulative. You may feel few effects with the first treatment. That will be great if it continues, but most likely gradually unpleasant side effects will set in. And when you know your chemo combo (it’s usually a combination of two chemo agents) go to “Chemocare.Com” and you will learn everything you need to know about the drugs and what it is supposed to be used for.
By week two after both my first series of treatments in 2013 and again in 2015, my hair began to come out. I had read that with TAXOL hair loss was a possibility. The first time was a bit more dramatic and I hoped that it would only be “thin”, but then it became so “scraggly” that I had my head shaved. So the second time around in 2015, I just had it shaved right away. My husband’s hair did NOT fall out!
I will tell you that summer definitely here and you should definitely stay OUT of the sun while in treatment. One of our cancer friends had a very badly sunburned arm. He had been driving with the window down and had his arm resting on the window. As much as I have always loved “basking in the sun”, I’m much more careful now.
Incidentally I consult with my oncologist each month. My husband is now in his 14th year of survival with no evidence of disease (NED). But at the beginning of the treatments and after the surgery return visits for follow-up were frequent, and gradually throughout the years the visits are now down to twice a year for my husband.
The second time around, during my treatments, I always went back the following day and had a hydration treatment, and also an injection of Neulasta. Neulasta helps keep your white blood cell count up so that your immune system is not so low that you become susceptible to germs more easily. It would be best to stay away from anybody who is sick. I also carry a small bottle of hand sanitizer in my purse. I use it all the time, especially after touching public bathroom doorknobs, grocery cart handles, etc. Yes, I’m germ conscious! Sometimes I have had to visit the Emergency Room. That is an unnerving experience when you’re in a room full of other sick people. I’ve feared catching something before I could get out of there, so I’m not beyond using a mask while I am in there.
Hydration is extremely important, because chemo has a way of draining the body of fluids and making one extremely weak. I was severely fatigued even more so the first time around because I didn’t “insist” on hydration following each treatment, nor did I get a Neulasta injection. But the “second time around” I “told” the doctor that I wanted hydration and a Neulasta injection after each treatment. He readily said, “No problem.”
Incidentally, it would be good if someone can accompany you when you go for consultations. When my husband and I would go for a consultation, I would take notes, so I could remember what we discussed during the visit. I ask questions, and even say, “How do you spell that?” Then I come home and do some research but only from reputable sources. When I went with my husband to his visits, I took notes. His first local surgeon frowned on our using a tape recorder. We asked him early on if we could use a recorder. He said, “Have you ever heard one of those things in court?” So we didn’t use it. But my oncologist is completely different. We turn on our camera and my husband does a video. I try to do that each time. It’s very helpful, and I always hear more the second time around than I did at the office. I took pictures and videos along the way during my husband’s treatment and surgery. If you wish to see some of them, I can send you a web link. They include lovely pictures of Pittsburgh, plus Dr. Luketich, and some “before and after” pictures of Bill.
Also my oncologist told me that I should keep something cold in my mouth for at least the first 24 hours after a chemo treatment. The chemo goes all over our bodies, and it can affect the teeth and gums. And so cold foods, popsicles, ice chips, etc. would be good. Avoid hot foods during that time period.
He also told me that rinsing my mouth often during the day with a baking soda solution would help keep my mouth moist. So I took a bottle of water (one teaspoonful of baking powder to 8 oz. of water) I kept one in each bathroom, and would rinse my mouth often during the day, and even when I would awake during the night. I never had mouth sores.
Okay with all that in mind these are things I did during my treatments. I’m sure others may have tips of their own, but these are things I found helpful. Incidentally, I think PRO-BIOTICS have helped me during my treatments. I like “Digestive Advantage” Probiotic fruit-flavored gummies made by Schiff. They are less expensive at a store like COSTCO. When they have a special sale, on I buy more than one bottle.
First, I took an anti-nausea pill each morning before breakfast. My nausea med was “Granisetron” (KYTRIL). I put a bottle of water and the pill on my night table, and when I first opened my eyes, I took that pill. I never had nausea. So that is like a pre-emptive strike—better taken before the nausea begins.
Secondly, I ate foods that were high in protein because that provides energy. I ate at regular times during the day, even if I wasn’t “hungry.” I ate cheese eggs and drank milk for breakfast. I also kept a protein count and wanted to be sure I consumed at least 60 grams of protein each day. Even then I was still “tired”. I still live with a good amount of fatigue but that’s because I still have cancer. At Stage IV, it isn’t going away. My prayer is that it will progress slowly.
Thirdly, I bought a container of “Performance Whey Isolate” from Costco in the vanilla flavor. Each serving provides 30 grams of premium whey protein, made exclusively from Isolate. My husband made me a “thick” milkshake consisting of vanilla ice cream, a scoop of whey, a big spoonful of peanut butter, and sometimes a Butterfinger candy bar all broken up prior to putting it in the glass. He put just enough milk (and that could be “half and half” for more calories, to make it like a soft ice cream that I ate with a spoon. I’ve never been fond of milk shakes, but some people love smoothies. This whey dissolves easily in whatever it is put in. It can be put in puddings as well. It comes in chocolate, vanilla and unflavored.
There is also BOOST that comes in different flavors that can be mixed with the whey & ice cream mixture. I also bought that at a box store. It comes in cases of 24 and has 15 grams of protein per bottle. It is less expensive when I buy a bigger quantity. Of course, it would be best to try one to see how you like it, before you buy a whole case of 24, naturally. It’s also necessary to drink as much water as possible during the day.
Although I haven’t used it, some oncologists recommend BENECALORIE if the patient is having a problem with weight loss. It is made by Nestle and can be purchased at Wal-Mart, I’m told. That’s a tip for those that are losing weight, which is not unusual during a chemo treatment. It is especially true if the patient is losing weight rapidly. I didn’t lose much weight during chemo, nor did my husband William.
Moving around as much as possible, and keeping up my regular daily routine was helpful. Our house is 184 feet from the street. It was all I could do to walk up and down the driveway two times. Perhaps extreme fatigue will not be your experience, but if it happens, it is normal.
As for Over the counter supplements, (OTC) they should be discussed with your doctor. I was Vitamin D deficient, so I took a Vitamin D tablet, and also a calcium tablet, as well as some fiber pills for regularity and a fish oil tablet. But needs will be different for different patients, depending on their medical problems, and I’m not saying you should take these, but adequate nutrition and hydration are ever so important.
So if you can maintain a normal daily routine as much as possible, going places, being with friends, and keeping a positive outlook will allow you to weather this storm much better. Even though a diagnosis like this turns your life upside down, it doesn’t mean that we can’t experience some “up” days. I hope you tolerate the treatments well, and that your tumor markers will be dramatically reduced. Once you have completed the treatments, you should begin to feel much better in a matter of a few weeks. At the end of treatments, you should have a repeat PET scan to determine the effectiveness of the treatments. And then if all is well, a surgery date will be set in approximately 3 weeks following your last chemo/radiation treatments. Chemo has a residual effect of 3 weeks even after the last treatment is given. And hopefully, you will be an excellent candidate for the Ivor Lewis Minimally Invasive Esophagectomy. (MIE) So “fasten your seat belts” and “we’ll cross that bridge when we get to it!”
And we’ll say a prayer for your 28-year old wife and your dear parents. By the way you’re the same age as some of my grandchildren. I’m old enough to be your grandmother at age 77 and ½. I’m now adding the “halves” back on because each passing day is another victory. And by the way, did I tell you I am often “brutally honest” in my desire to be upfront with those that are diagnosed with cancer of any kind! So if I sound “bossy” that’s because I think the “young ones” are always in need of good counsel, and I haven’t lived this long without learning something. I’ve earned my “now” silver strands among the gold hair!
All the best,
Loretta (Wife of William, EC Stage III (T3N1M0) MIE @ UPMC on May 17, 2003 by Dr. James D. Luketich)
______________________________________________________________
(My note: There are different tumor markers for Ovarian cancer than for Esophageal Cancer. My husband is seen by our oncologist twice yearly and a CBC is taken, and a PET/CT scan or a CT scan is performed on at least a yearly basis. But if something happened during the year, naturally we would just call the oncologist and he would schedule the necessary tests or scans depending on the nature of the problem.)
“…How are tumor markers measured?
A doctor takes a sample of tumor tissue or bodily fluid and sends it to a laboratory, where various methods are used to measure the level of the tumor marker.
If the tumor marker is being used to determine whether treatment is working or whether there is a recurrence, the marker’s level will be measured in multiple samples taken over time. Usually these “serial measurements,” which show whether the level of a marker is increasing, staying the same, or decreasing, are more meaningful than a single measurement…
“CA19-9
- Cancer types: Pancreatic cancer, gallbladder cancer, bile duct cancer, and gastric cancer
-
Tissue analyzed: Blood
-
How used: To assess whether treatment is working…
Carcinoembryonic antigen (CEA)
- Cancer types: Colorectal cancer and some other cancers
-
Tissue analyzed: Blood
-
How used: To keep track of how well cancer treatments are working or check if cancer has come back…”
_________________________________________________________
“Whether you're preparing for your chemotherapy journey or managing
the side effects, we have the information you need...every step of the way.Just getting started? New to Chemotherapy is the place to start “
_________________________________________________________
3. https://medlineplus.gov/cancerchemotherapy.html
“…Normally, your cells grow and die in a controlled way. Cancer cells keep forming without control. Chemotherapy is drug therapy that can kill these cells or stop them from multiplying. However, it can also harm healthy cells, which causes side effects.
During chemotherapy you may have no side effects or just a few. The kinds of side effects you have depend on the type and dose of chemotherapy you get. Side effects vary, but common ones are nausea, vomiting, tiredness, pain and hair loss. Healthy cells usually recover after chemotherapy, so most side effects gradually go away.
Your course of therapy will depend on the cancer type, the chemotherapy drugs used, the treatment goal and how your body responds. You may get treatment every day, every week or every month. You may have breaks between treatments so that your body has a chance to build new healthy cells. You might take the drugs by mouth, in a shot or intravenously.
NIH: National Cancer Institute…”
________________________________________________________
4.
 https://www.youtube.com/watch?v=vKIRWY-LMYc
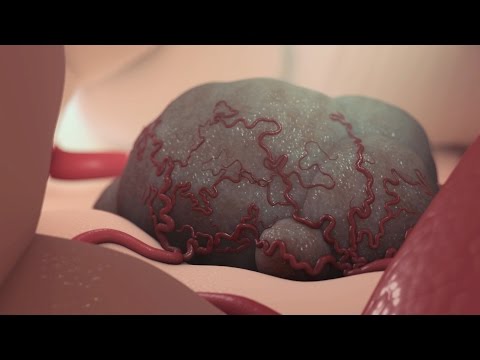
https://www.youtube.com/watch?v=vKIRWY-LMYcAnimated video explaining how chemotherapy works
Published on Jul 27, 2012 -
“This video about chemotherapy, created by Nucleus Medical Media, depicts normal cell division, apoptosis, tumor cell formation, tumor development, and angiogenesis of a tumor. It describes the cause of tumor cell formation at the genetic level with DNA, and metastasis through blood and lymph vessels. This animation covers the various effects of chemotherapy: cancer cell death, tumor death, destruction of normal cells and tissue. It also covers the side effects associated with chemotherapy treatments. Also described are related treatments, such as, radiation, pills, capsules, liquids, intravenous injections, surgical procedures, catheterization, CSF injection, wafer placement, and schedule of treatments.”
___________________________________________________________
5.
 https://www.youtube.com/watch?v=gQwIPFGXSKg
https://www.youtube.com/watch?v=gQwIPFGXSKgThis is a 56 minute lecture on chemotherapy and its effects on the body
Uploaded on Feb 3, 2011
Get the notes: http://www.lulu.com/product/paperback...
The lecture notes for this and all numbered lectures are available at Lulu.com, keyword PHRM203 or just follow the link. The notes do NOT include Exam Reviews, Paramedic Pharm, Heart Sounds, or Chest Tubes.____________________________End of references________________
-
"mister"~FYI - Esophageal Cancer diagnoses & stages & gradesmister_eko said:guys, thank you all so much
guys, thank you all so much for chiming in. I do feel much better. Where would you suggest I go looking for other treatment options? So far, I know about HER2 and Immuno Oncology, but doctors told me both would be options should chemo, radiation and surgery don't kill it completely
I got a second opinion form Piedmont Hospital which is a part of Md Anderson group and they agreed with Emory. Emory also has the best surgeon for this type of cancer, dr. SeTh Force.
Dear “mister_eko”
You asked what stage my husband’s cancer was. The diagnosis was Adenocarcinoma @ the Gastroesophageal (GE) junction, Stage III (T3N1M0). Below my name you will see how those stages break down. By the way, there are two types of Esophageal Cancer, SQUAMOUS and ADENOCARCINOMA. What is your exact diagnosis and for which type of Esophageal Cancer?
You need to understand what is taking place inside your body so you can interact intelligently with your doctors. And I will be sending you a separate letter with more references. However, this “Cancer.net” site is a great in-depth site that thoroughly explains Esophageal Cancer.
Also, I know you’re starting chemotherapy this week. What types of chemotherapy drugs will you be having? And by the way, have you been tested for HER2 (human epidermal growth factor receptor 2) to see if you have the over-expressive cell that causes the cancer to spread more rapidly? If you test “positive”, you should be receiving HERCEPTIN in addition to any chemo drugs you are taking. It is given alongside the chemo although in itself it is not a chemo drug. Herceptin is now approved for both Breast cancer (BC) and Esophageal Cancer (EC) patients. At first it was thought that this particular cell was found only in BC patients, but it was later found to be prevalent in Gastric cancer patients as well. And so the FDA has approved the use of HERCEPTIN for those who test positive for this rapidly-dividing cell.
For your info, here was my husband’s schedule when he was having his pre-op (neo-adjuvant) chemo/radiation treatments.
_____________________________________________________________
William’s treatment schedule was as follows:
Week 1 ~ (02-10-03) Chemo 96-hr. continual infusion of Carboplatin/5-FU (via Fanny pack)
Weeks 2, 3, and 4 ~ (02-17-03) Five days-a-week radiation treatment. (No CyberKnife equipment (targeted radiation) in this area in 2003, but now we do have one in our Tidewater area.)
Week 5 ~ Combination radiation plus SECOND chemo continuous 96-hr. infusion (via Fanny pack)
Week 6 ~ (03-17-03) Final week of radiation.
Repeat PET Scan on 04-28-03 ~ results - COMPLETE ERADICATION OF TUMOR in Esophagus and the 2 affected lymph nodes.
Laparoscopic surgery was scheduled for May 17, 2003 at the University of Pittsburgh Medical Center (UPMC) by the pioneer of the Ivor Lewis Minimally Invasive Esophagectomy (MIE) Dr. James D. Luketich, approximately 3 weeks later after successful pre-op treatment. Radiation does cause scar tissue, so the sooner the surgery after the pre-op treatments—the better.
_________________________________________________________
Hope this information will be helpful for you. Incidentally, I’m suggesting that you keep a JOURNAL of your doctor’s visits, chemo treatments and the side effects you felt at the time you received them, etc. You should be asking for a printed copy of all your medical treatments at the time you receive them, or as soon after as possible. Also when you are having a scan of any type, inform the person doing the testing that you would like a personal copy of the disc for your own medical records. It will be given to you at no charge. That way when you go for a second opinion, you won’t have to make trips back to all the places you’ve been gathering up records. And I will be giving you some “rankings” in another letter about PIEDMONT, as well as EMORY. Personally, I would not consider a 2nd opinion at “Piedmont” as a bonafide second opinion. They are not “cancer specialists!”
Sincere best wishes for all the days that follow,
Loretta
P.S. I will be sending you via a separate post tips that were helpful for me when I had my chemo treatments consisting of Carboplatin and Paclitaxel (Taxol). However, William’s chemo consisted of Carboplatin and 5-FU. I have found the Chemocare.com website information to be invaluable.
1. http://chemocare.com/chemotherapy/drug-info/
Simply find the name of the chemo that you’re receiving and it will tell you everything you need to know about that particular drug. It will also tell you about side effects, and helpful hints on how to manage certain side effects. As for me, my main symptom was extreme fatigue. But I will send you a separate letter sharing some tips for you that were helpful for me.
_______________________________________________________
2. <
-
Hi, I'm lisa.. 37yr old
Hi, I'm lisa.. 37yr old female. I just had my ercp and colonoscopy and the Dr took 15 biopsies. Have struggled with heartburn for about 6 yrs. Have an annoying hiccup issue everyday, but it is just a single one that is very loud. I'm on here trying to learn more as I'm a bit scared now and not sure what to think. Also was told I am in beginning stage liver failure due to a genetic disorder. My father had liver failure and received his transplant 4 years ago but now he has 2 neuroendocrine gastrinomas, where the cancer has spread to 3 of the lymph nodes. Anyone have family history of liver cancer ? My dad swears his only sign through the years was constant heartburn and esophagus issues.
-
Lisa~U R wise 2 begin search 4 INFO AFTER U KNOW the diagnosis
Good afternoon Lisa
We gladly welcome your inquiry here. Although most of the entries here begin with a patient who has been diagnosed with Esophageal Cancer. Most often it came as a result of difficulty swallowing and a history of heartburn. Now you did mention “one hiccup”. When my husband and I went to our internist, we told him we were there because my husband was having a hiccup each time he began to eat. He would have only one hiccup, but no difficulty swallowing. Our doctor said he had no idea what the problem was but he scheduled an Endoscopy with a gastroenterologist. So in two days we learned that my husband has Esophageal Cancer. Now I don’t need to go into detail here about his stage, grade and treatment here for EC. I don’t think you need to go that far at this point. Moreover, most patients here whose “primary” diagnosis is Esophageal Cancer do often have metastasis to the Liver.
However, since you say you been told that you are “in beginning stage liver failure due to a genetic disorder”, it seems that most likely you are not going to be diagnosed with Esophageal Cancer. It sounds as if you may well have problems similar to your father’s, but please don’t take my words as any kind of diagnosis. I can speak intelligently on the subject of Esophageal Cancer, but have no experience with “Gastrinomas”.
However when I looked up the meaning of “ERCP” and found it to be this. “Endoscopic retrograde cholangiopancreatography (ERCP)—pronounced “[ko-lan″je-o-pan″kre-ah-tog´rah-fe] -- a test used to find and treat abnormalities in your pancreas, bile ducts, and gallbladder. ERCP is a combination of two tests: an endoscopy and an X-ray. I see that it is a thin tube with a small camera that is “threaded down your Gastrointestinal tract. Your GI tract consists of your esophagus, stomach, and intestines.
You say the doctors took 15 biopsies. Lisa, from what you describe, it seems that whoever your team of medical doctors are has performed some extensive testing. And since the lighted tube with the camera has taken pictures of your Esophagus, if there are tumors in the Esophagus, they will surely be noted in the doctor’s report, which I’m assuming is “YET FORTHCOMING.”
So while I know it is “normal” to run ahead of the doctors and diagnose oneself, all I can say is to “brace yourself” for what might be forthcoming. However, from the explanation of your father’s diagnosis, it seems that this condition is “genetic” and that problems lie more in your Liver than in your Esophagus. But understand I have no “medical training”, only personal experience with Peritoneal, Ovarian and Esophageal Cancer. So I certainly understand your level of anxiety, and it is not at all uncommon to be “worried sick” wondering about your problems. CANCER is one of the “scariest” words in our English language. When we first heard the audible words spoken back in 2002, by the gastroenterologist, “Your husband has cancer” we interpreted them inwardly. Our “emotions” heard, “You are going to die!” Don’t know about others but that was our first immediate reaction. That sent us on a search to find out what Esophageal Cancer is all about. Fast forward to August 2016, my husband was blessed to be a candidate for his Stage III EC (T3N1M0), and he is in his 14th year of survival with no evidence of disease. (NED) So even when one is actually diagnosed with EC, we always pray that they will be able to have successful treatments and survive.
If you are presented with a diagnosis of Esophageal Cancer, however, you can reference my reply to mister_eko, where you can review a series of tests and stage explanations for EC.
http://csn.cancer.org/comment/1548791#comment-1548791
Ask the doctors plenty of questions. And no matter what you suspicion your problems to be, with the medical history of your father, I would certainly want a SECOND OPINION. As is the case so often, “newbies” do not include any background info as to where they are being treated and/or why they sought treatment in the first place.
When I read your letter, I had to go to the dictionary to find out what an “ERCP” is and it’s no wonder you just put in the abbreviation. Here is the long version of “ERCP” -- “cholangiopancreatography” - [ko-lan″je-o-pan″kre-ah-tog´rah-fe]. See references below for more about what those tests involves and more about Gastrinomas.
So for the time being, I can sympathize with you, but speaking for myself, I really cannot help you at this time other than to share with you some references that I have found that help me to understand what you might be facing. Perhaps they might help you as well. I am extremely sorry that both you and your father are joining our family of “fellow sufferers with diagnoses we wish we never heard of!”
Please write again if you think I can help. Others may join in welcoming you and know more than I can offer. If so they will be answering you as well. I just wanted you to know that we know you’re here and now you know we’re here if we can help.
Sincerely,
Loretta Marshall (wife of William who was first diagnosed with EC in 2002 and is still surviving, thank God!
____________________________________________________________________
So, Lisa, bottom line for now is that you are wise to begin to familiarize yourself with reputable medical sites that deal with Gastrointestinal conditions as a specialty.
1. http://www.healthline.com/health/ercp?utm_source=ask&utm_medium=referral&utm_campaign=asksearch#Overview1
“What Is ERCP?
Highlights
ERCP is a procedure used to find and treat problems in your pancreas, bile ducts, and gallbladder. It combines an endoscopy and an X-ray.
During the procedure, a thin tube with a small camera attached to the end is threaded down your gastrointestinal tract. Dye is injected to help any abnormalities show up on the X-ray images.
ERCP is generally a safe procedure and most people experience no complications.
Endoscopic retrograde cholangiopancreatography (ERCP) is a test used to find and treat abnormalities in your pancreas, bile ducts, and gallbladder. ERCP is a combination of two tests: an endoscopy and an X-ray.
An endoscopy is a procedure in which a thin, flexible tube attached to a tiny camera is threaded down to your gastrointestinal (GI) tract. Your GI tract consists of your esophagus, stomach, and intestines.
This camera will be used to take an X-ray of the insides of your bile ducts and pancreatic ducts. Your bile ducts are also sometimes called biliary ducts. The ERCP can help your doctor find and treat any blockages in these ducts. The results will also help them diagnose the reason for the blockage…”
____________________________________________________________
In reference to your father’s present condition here is an explanation of what he is dealing with. This may be “old” info for you, but I have to research words I have never heard before. So this is info for me, and anyone else who didn’t know what a “gastrinoma” was all about.
1. http://www.surgery.usc.edu/divisions/tumor/pancreasdiseases/web pages/Endocrine tumors/pancreatic tumors/gastrinoma.html
“What is a gastrinoma
Gastrinomas are rare endocrine tumors and commonly present with severe recurrent peptic ulcer disease. More than 60% of gastrinomas are cancerous and the tumor eventually spreads to the liver and other parts of the body.
How are gastrinomas diagnosed?
A diagnosis of a gastrinoma should be considered in a patient with peptic ulcers that recur frequently and are resistant to treatment. A biochemical study to measure the level of gastrin and its response to a hormone called secretin is utilized to make the diagnosis.
Once a diagnosis is made, localizing the tumor is important. Most gastrinomas are small lesions and therefore, localizing the tumor may be difficult. Some of the tests that are performed to localize the tumor include a CT scan, octreotide scan and MRI and an endoscopic ultrasound.
An experienced surgeon will detect these tumors at surgery even when they are not visible on preoperative imaging tests…”
2. http://www.yourhormones.info/endocrine_conditions/gastrinoma.aspx
Gastrinoma
“Gastrinomas are tumours that are usually found in the first part of the small intestine or in the pancreas that produce large amounts of the hormone gastrin.
Alternative names for gastrinoma
Zollinger-Ellison syndrome; Z-E syndrome; ZES
What are gastrinomas?
Gastrinomas are tumours that produce large quantities of the hormone gastrin which stimulates the production of gastric acid in stomach. Most of these tumours are found either in the duodenum (first part of the small intestine) or the pancreas. Rarely these tumours have been found in the stomach, bile duct, liver, ovaries and heart. Gastrinomas of the pancreas are usually larger in size (average 3-4 cm) and are commonly associated with spread to the liver (20-25% cases) and adjacent organs at the time of diagnosis, as compared to gastrinomas of the small intestine which are usually smaller (<1cm) and less likely to spread to the liver (5-10% cases).
What causes gastrinomas?
Gastrinomas arise due to uncontrolled division and replication of specialised G cells which produce the hormone gastrin. The exact trigger for the uncontrolled growth of these cells is not known. Genetic mutations are believed to play a part in development of these tumours.
What are the signs and symptoms of gastrinomas?
The signs and symptoms of gastrinomas are related to increased gastric acid production by the tumour cells. Most patients experience abdominal pain, heartburn, nausea, blood in the vomit, bleeding from the back passage and diarrhoea. On average these symptoms are present for five years prior to a definitive diagnosis of gastrinoma being established.
Gastrinomas may be present in 0.1% of patients who have ulcers in their stomach or small intestine. The diagnosis of gastrinoma should be suspected in patients with stomach or small intestinal ulcers if they:
are resistant to treatment - have recurrent disease - have associated complications such as intestinal perforation and bleeding - have high calcium levels - have a family history of multiple endocrine neoplasia type 1 syndrome which is an inherited condition affecting multiple glands such as the pituitary, pancreas and parathyroid glands…
· What are the longer-term implications of a gastrinoma?
In cases where the tumour has not spread to any adjacent organs and has been successfully removed by surgery, patients should go on to lead full and active lives. Patients treated with surgery will need to attend regular hospital checks to assess for recurrence of the tumour using blood tests or radiological investigations. Gastrinoma, if left untreated, can lead to ulcers, perforation and bleeding from the small intestine. Jaundice and weight loss may also occur as a result of these tumours spreading to the liver. These tumours are usually slow growing and proton pump inhibitors are highly effective in controlling the symptoms where surgery is not possible…”
________________________________________________________________
I find the Mayo Clinic to be a good “user friendly” site that is more understandable than sites with numerous medical terms that are not easily defined and consequently more difficult to understand. But I have included two references relative to Liver cancer and Gastrinomas. You may want to research them further.
3. http://www.mayoclinic.org/diseases-conditions/liver-cancer/diagnosis-treatment/diagnosis/dxc-201981764. http://www.mayoclinic.org/search/search-results?q=gastrinomas
I also find this “UK” site to be extremely good at explaining conditions and treatments on many different topics. And well they should be because the UK has universal health care. In corresponding with patients from the UK and Canada in the past, I find that they are not always eligible for tests and treatments that we have in the US today. So the more defining info that can be placed on the web for UK patients, I say all the better.
5. http://www.cancerresearchuk.org/about-cancer/cancers-in-general/cancer-questions/gastrinomas
“Gastrinoma
This page is about gastrinoma, a rare type of neuroendocrine tumour that usually develops in the gut (digestive system). There is information about
What gastrinomas are
Gastrinomas are rare tumours that usually start in the gastrin producing cells in the small bowel (duodenum) or pancreas.
Gastrin is a hormone that controls the amount of acid in the stomach. Acid helps to digest food. Gastrinomas produce large amounts of gastrin and this causes the stomach to make more acid. Too much acid leads to ulcers in the stomach and small bowel. The combination of high gastrin levels, too much stomach acid, and severe ulcers is called Zollinger Ellison Syndrome (ZES)…”
_______________________End of references___________________
-
My husband who just turned 65
My husband who just turned 65 in April was diagnosed with esophagial cancer last week. Today after having a CAT scan and PET scan we learned he has an 11 centimeter tumor at the base of his esophagus and there are lymph nodes affected by no organs. He is scheduled for chemo next week - 2 days a week every other week. He's strong but I just read the possible side effects of the 3 drugs they wants to use and it's truly frightening - not only this cancer but the side effects. He may also have the Her2 protein present which is good according to the oncologist because there is another drug, Herceptin, that targets this particular protein and can shrink the tumor. I'm not sure why I'm writing all this -- maybe it's part of my therapy/acceptance of what has just been found out about my husband's health. Yet, maybe a month ago he had a complete physical and was told to keep doing what he's doing cause all looks good. He complained abouto acid reflux, had an endoscopy and there it was this 11 centimeter (approx 5 inches) tumor. We are both still in disbelief to a degree. I don't know hat to do now.
-
Take things one day at a time and find a good surgeon
Angela,
I was 61 years old when I was diagnosed with esophageal cancer. Like your husband, I was feeling fine and had recently had a physical where all seemed normal. I went in to see my doctor to get a prescription for omeprazole because I was tired of waking up in the middle of the night with heart burn. My doctor said “Let’s do an endoscopy just to be safe”. When the GI doctor who did the endoscopy called me to tell me they found a tumor I was shocked. For a while I kept thinking maybe they had the wrong test results and the next test I had was going to show that everything was fine.
The good news is that esophageal cancer can be treated with chemotherapy, radiation therapy, and surgery. Admittedly the surgery is extensive. I always suggest to newly diagnosed patients, that they seek a second option of a surgeon at a major cancer center that specializes in esophageal cancer.
For now the best approach is to take one day at a time and focus on the things that need to be accomplished in the immediate future. There will be a whole series of tests to complete staging, followed by treatment and a whole series of tests to check the results of those treatments.
The side effect descriptions of the agents used for chemotherapy can sound daunting, but modern day oncology has defined a number of medical interventions for minimizing and dealing with those side effects. I am not trying to suggest that chemotherapy and radiation therapy is a “walk in the park”; but it is survivable, and not all patients experience all the side effects. Some patients experience very few side effects. In my personal experience I experienced some of the side effects but my oncologist gave me other medications to mitigate the side effects.
HER2 positive can be a good thing. Herceptin is a targeted drug that seeks out cells that exhibit the specific protein, it is therefore a “targeted” treatment, unlike many of the other chemotherapy agents that are just designed to seek out and destroy rapidly reproducing cells. Standard chemotherapy agents that attack rapidly reproducing cells kill cancer but they also attack other rapidly reproducing cells like those in hair, nails, the mouth, and digestive system. The drug protocols for treating esophageal cancer as pretty standard. Here is a reference that describes staging and standard treatment approaches:
https://www.nccn.org/patients/guidelines/esophageal/index.html
Finding an experienced surgeon is very important.
Tell your husband this is going to be a tough year, but there is life after cancer diagnosis. He is relatively young and with a good health profile he has the strength to complete treatment. It has been almost 7 years since my treatment and surgery, and so far I have been fortunate to have clear scans and checkups. I am back to doing the things I enjoy with the people I love.
Wishing you both the best on your journey to eradicate this cancer.
Best Regards,
Paul Adams
McCormick, South Carolina
DX 10/2009 T2N1M0 Stage IIB - Ivor Lewis Surgery 12/3/2009
Post Surgery Chemotherapy 2/2009 – 6/2009 Cisplatin, Epirubicin, 5 FU
Six Year Survivor
-
Angela~U will find help & acceptance here-Glad U wrote!AngelaMarsh said:My husband who just turned 65
My husband who just turned 65 in April was diagnosed with esophagial cancer last week. Today after having a CAT scan and PET scan we learned he has an 11 centimeter tumor at the base of his esophagus and there are lymph nodes affected by no organs. He is scheduled for chemo next week - 2 days a week every other week. He's strong but I just read the possible side effects of the 3 drugs they wants to use and it's truly frightening - not only this cancer but the side effects. He may also have the Her2 protein present which is good according to the oncologist because there is another drug, Herceptin, that targets this particular protein and can shrink the tumor. I'm not sure why I'm writing all this -- maybe it's part of my therapy/acceptance of what has just been found out about my husband's health. Yet, maybe a month ago he had a complete physical and was told to keep doing what he's doing cause all looks good. He complained abouto acid reflux, had an endoscopy and there it was this 11 centimeter (approx 5 inches) tumor. We are both still in disbelief to a degree. I don't know hat to do now.
Hi Angela,
In case you didn’t know, you’ve come to a good place for understanding and good information. It will be “therapeutic” both acceptance-wise and information-wise. So although I know this is a letter you wish you never had to write, and still probably can’t even believe that it is real at this point. But believe it quickly, accept it and research this cancer thoroughly. It will give you confidence that your husband is receiving the very best of care.
When I am facing some new problem, I want to first know if I am the only one going through this, or if there are others who have gone through this before me. And you will find several of us here who have "been there--done that."
And I always ask, "What is the one thing I don't want to do, and what is the thing I definitely SHOULD DO?" So my top advice is always to have a SECOND OPINION at a hospital that specializes in the Ivor Lewis MINIMALLY INVASIVE ESOPHAGECTOMY (MIE).
You have described a diagnosis similar to that of my husband. His was termed "Adenocarcinoma at the GastroEsophageal junction). His diagnosis was EC Stage III (T3N1M0). That meant that the tumor had penetrated all 4 walls of his Esophagus and also had spread to 2 local lymph nodes. The "T" stands for tumor and how far it has spread. The "N" stands for "node" and each number corresponds to how many lymph nodes are affected. The "M" stands for metastasis, and that was a "ZERO" because there was no spread near or in another major organ. So by what you describe, it appears that your husband will be able to qualify for an Esophagectomy. Since you say the tumor is at the base of his Esophagus, this would be termed Adenocarcinoma at the Gastroesophageal junction (GE). (11 centimeters is equal to 4.330709 inches)/
Not all Esophagectomies are performed in the same manner, and not all Thoracic Surgeons are "equally-skilled" in the performance of esophagectomies! Because it is so late tonight, I will not write my usual detailed letter. Fright, shock, uncertainty, bewilderment, and sadness are usual emotions that accompany a cancer diagnosis. But be encouraged, it does not mean it's the end of your and your husband's world. You're entering a long and seemingly-dark tunnel, but the light at the other end isn't always another oncoming train. There are survivors here that are only too eager to help you along the way.
Wishing you and your husband every success,
Loretta Marshall (Wife of William) first diagnosed at age 66 in 2002, and underwent a successful MIE by Dr. James D. Luketich at the University of Pittsburgh Medical Center (UPMC) May 17, 2003 and is alive and well today.
-
Discussion Boards
- All Discussion Boards
- 6 Cancer Survivors Network Information
- 6 Welcome to CSN
- 122.7K Cancer specific
- 2.8K Anal Cancer
- 457 Bladder Cancer
- 313 Bone Cancers
- 1.7K Brain Cancer
- 28.6K Breast Cancer
- 407 Childhood Cancers
- 28K Colorectal Cancer
- 4.6K Esophageal Cancer
- 1.2K Gynecological Cancers (other than ovarian and uterine)
- 13.1K Head and Neck Cancer
- 6.4K Kidney Cancer
- 685 Leukemia
- 805 Liver Cancer
- 4.2K Lung Cancer
- 5.1K Lymphoma (Hodgkin and Non-Hodgkin)
- 243 Multiple Myeloma
- 7.2K Ovarian Cancer
- 71 Pancreatic Cancer
- 494 Peritoneal Cancer
- 5.7K Prostate Cancer
- 1.2K Rare and Other Cancers
- 544 Sarcoma
- 744 Skin Cancer
- 662 Stomach Cancer
- 194 Testicular Cancer
- 1.5K Thyroid Cancer
- 5.9K Uterine/Endometrial Cancer
- 6.4K Lifestyle Discussion Boards



