The Cancer Survivors Network (CSN) is a peer support community for cancer patients, survivors, caregivers, families, and friends! CSN is a safe place to connect with others who share your interests and experiences.
Update Kidney Cancer Treatments
Comments
-
old statsGSRon said:Stats lie..
Those stats do lie.. as others have said.. they are old and do not take in to account all that has been learned since those stats were printed. In fact, if you can read this.. then you are reading a posting from a ghost..! Oh wait.. I am real and alive...! Many of us have passed the stats... me included... and I plan to be here a long time...
Practice for the TT Races start in less than an hour... life is good..!!
Cheers.!
Ron
are not nearly accurate to the stats you would find from just over the past year. Too many of us are doing real well.
-
Could you name some? Or tell where the info came from?todd121 said:Could you name some? Or tell where the info came from?
Could you please name some of the drugs studied, or maybe name some of the studies? Or tell me where to look? I'd like to see these papers.
I was under the impression that the new drugs like Votrient and Everolimus and some of the others were so new, and it takes so long to do these studies (5-10 years), that there were no completed studies.
I'm interested in knowing which drugs were studied and how, and for how long, etc. I'd like to see the papers.
Or could you tell me where you got the information? Are you relaying information your oncologist told you?
I would hope if they've found negative benefits, it shouldn't be ethical to continue to study similar drugs and they wouldn't do it. Unless the negative benefit was so slight that it wasn't clear if it was neutral or negative....
Thanks,
Todd
Todd, perhaps I can save him the trouble. I've referred you to these materials before, summarised the outcome before and also explained the rationale for having low expectations of success, previously. This time I'll go further, detail a good source and quote some key excerpts.
The whole matter was given a good going over at the 2012 KCA National Patients Conference at MDAnderson in Texas. This topic was comprehensively covered by Chris Wood, by common consent the best onco-urological surgeon in the World. Peggy Zuckerman from California (who has paid a very occasional visit here, was one of the key participants on KIDNEY-ONC and now is on Smart Patients) performed a great service for us all in reproducing most of that Conference's proceedings, together with the slides at her excellent WordPress blog which you might care to explore. There's days/weeks of reading there so I'll point you to the part relevant for present purposes, viz:
http://peggyrcc.wordpress.com/2012/06/
Since there's a vast amount of material there, I'd recommend that you scroll to the bottom of that entry and then back up to find the first of Chris Wood's four talks: Locally Advanced RCC/Kidney Cancer; Dr. Chris Wood; Options & Treatment 1/4 Parts
You'll find a lot of good stuff there. I promised a few key quotes, so here goes:
Adjuvant Therapy means some form of therapy– chemo, radiation, vaccine, whatever–after complete surgical tumor resection with the idea to decrease the risk of recurrence of disease. The benefit is that the patient has already had surgery before getting additional therapy, but the downside is that many of those patients may have been cured by the surgery and they may get treatment they don’t really need.
That was the point I made to you when you were first contemplating entering the EVEREST trial. He goes on to present a very clear and intelligent analysis of this field. The use of all adjuvant treatments prior to the targeted therapies is dismissed easily:
Adjuvant Therapy: 2012
A variety of trials have been performed. Many patients have participated. They include radiation, embolization, energy ablation, a variety of different hormonal therapies, immunotherapies with interferon and interleukin 2, all having been used in an adjuvant setting. There have been a variety of vaccines preparations and we did a Phase III trial of thalidomide trial here. To date, not one of these therapies has shown benefit in the adjuvant setting. In fact, many of the patients on the treatment arms did worse than those who were not treated.
Then we get to the nub of your question
What about targeted therapies? That is also the great unknown where things stand with targeted therapies in the adjuvant setting.
Since 2006 there have been seven new agents against kidney cancer. It’s been a revolution. And to be honest, many have benefited from that advance. How do we use these agents in the context of adjuvant therapy?
There is a variety of trials recently completed or in accrual, ongoing. Tthe ARISER Trial used an antibody called G250 against Carbonic Anhydrase IX, and patients were randomized to get either antibody or placebo. This trial completed accrual many years ago, in fact, and we are still awaiting results which leads me to believe that is probably going to be a negative trial.
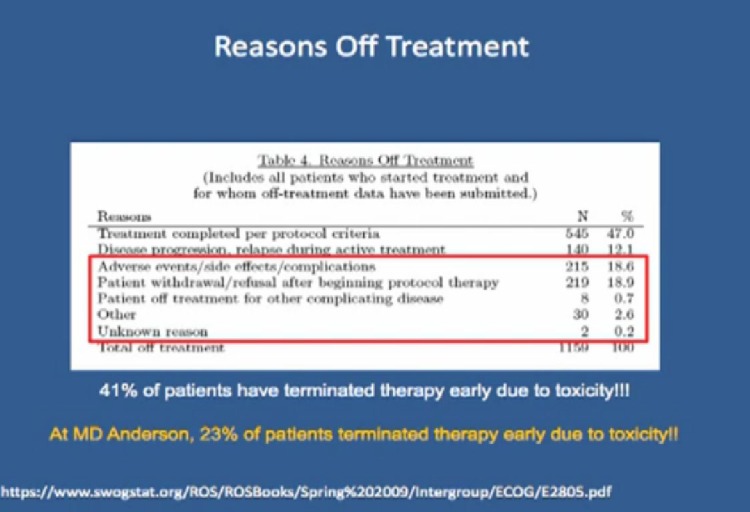
One thing that we did learn from this trial is that tolerance for the toxicity associated with targeted therapy in the adjuvant setting is not the same as in the metastatic setting. In this trial 41% of patients stopped therapy early, not because disease returned, or because they finished, but because of toxicity. I think it comes down to an individual assessment of the risks. If I told you that you have a 20% risk of your cancer coming back, versus your 70% chance of your cancer coming back and you are miserable on this therapy, all of a sudden 20% doesn’t look so bad.
He goes on to discuss various trials, including the ASSURE trial they conducted of which he says:
One thing that we did learn from this trial is that tolerance for the toxicity associated with targeted therapy in the adjuvant setting is not the same as in the metastatic setting. In this trial 41% of patients stopped therapy early, not because disease returned, or because they finished, but because of toxicity. I think it comes down to an individual assessment of the risks. If I told you that you have a 20% risk of your cancer coming back, versus your 70% chance of your cancer coming back and you are miserable on this therapy, all of a sudden 20% doesn’t look so bad.
My concern about this, because at the end of the day, if this trial matures and it is negative, will it be negative because the agents did not work, or because the patients could not tolerate the side effects. And too many patients stopped the trial early or had dose reductions. I’m afraid it is not going to be interpretable.
Aside from the theoretical reasons for supposing that none of these agents CAN be expected to work as adjuvants, this issue of interpretability may well sink all of these attempts. He goes on to observe that it's anybody's guess whether any of these trials and nay of these drugs will even have any relevance by the time the jury's finally in! All, we hope, will have been superseded by then by much more effective treatments.
Some time has elapsed since the work he was reporting on. From the recent AVEO tivozanib fiasco, we see, writ large, the non-feasability of carrying through these trials in the US. Recruitment problems are also at present looking almost insuperable in the UK. Meantime, there don't seem to be any preliminary findings of success from any of these trials, whether completed or still ongoing.
You will, I'm sure, readily appreciate many of these issues since you're encountering the problems at first hand and, as you'll read, you would be far from the first to drop out of a trial before completion, if you decide not to stay the course.
[On a purely personal note, I'm confident you'll forgive me if I pass a comment about your situation. In your shoes, I would be carefully weighing the hypothetical benefits of being in the trial against the compromise of my lifestyle. If you are on an agent which is immunosuppressive and which prejudices your daily activities via the unpleasant side-effects, you might be better off if you were feeling well and able to devote yourself, rather, to optimising your lifestyle - diet, regular exercise, meditation, etc? If the effects of the trial are undermining your general health care while holding out purely putative benefits, you might be better off not in it?]
As you are wont to say, 'I hope this helps'.
-
Texas is rightTexas_wedge said:Could you name some? Or tell where the info came from?
Todd, perhaps I can save him the trouble. I've referred you to these materials before, summarised the outcome before and also explained the rationale for having low expectations of success, previously. This time I'll go further, detail a good source and quote some key excerpts.
The whole matter was given a good going over at the 2012 KCA National Patients Conference at MDAnderson in Texas. This topic was comprehensively covered by Chris Wood, by common consent the best onco-urological surgeon in the World. Peggy Zuckerman from California (who has paid a very occasional visit here, was one of the key participants on KIDNEY-ONC and now is on Smart Patients) performed a great service for us all in reproducing most of that Conference's proceedings, together with the slides at her excellent WordPress blog which you might care to explore. There's days/weeks of reading there so I'll point you to the part relevant for present purposes, viz:
http://peggyrcc.wordpress.com/2012/06/
Since there's a vast amount of material there, I'd recommend that you scroll to the bottom of that entry and then back up to find the first of Chris Wood's four talks: Locally Advanced RCC/Kidney Cancer; Dr. Chris Wood; Options & Treatment 1/4 Parts
You'll find a lot of good stuff there. I promised a few key quotes, so here goes:
Adjuvant Therapy means some form of therapy– chemo, radiation, vaccine, whatever–after complete surgical tumor resection with the idea to decrease the risk of recurrence of disease. The benefit is that the patient has already had surgery before getting additional therapy, but the downside is that many of those patients may have been cured by the surgery and they may get treatment they don’t really need.
That was the point I made to you when you were first contemplating entering the EVEREST trial. He goes on to present a very clear and intelligent analysis of this field. The use of all adjuvant treatments prior to the targeted therapies is dismissed easily:
Adjuvant Therapy: 2012
A variety of trials have been performed. Many patients have participated. They include radiation, embolization, energy ablation, a variety of different hormonal therapies, immunotherapies with interferon and interleukin 2, all having been used in an adjuvant setting. There have been a variety of vaccines preparations and we did a Phase III trial of thalidomide trial here. To date, not one of these therapies has shown benefit in the adjuvant setting. In fact, many of the patients on the treatment arms did worse than those who were not treated.
Then we get to the nub of your question
What about targeted therapies? That is also the great unknown where things stand with targeted therapies in the adjuvant setting.
Since 2006 there have been seven new agents against kidney cancer. It’s been a revolution. And to be honest, many have benefited from that advance. How do we use these agents in the context of adjuvant therapy?
There is a variety of trials recently completed or in accrual, ongoing. Tthe ARISER Trial used an antibody called G250 against Carbonic Anhydrase IX, and patients were randomized to get either antibody or placebo. This trial completed accrual many years ago, in fact, and we are still awaiting results which leads me to believe that is probably going to be a negative trial.
One thing that we did learn from this trial is that tolerance for the toxicity associated with targeted therapy in the adjuvant setting is not the same as in the metastatic setting. In this trial 41% of patients stopped therapy early, not because disease returned, or because they finished, but because of toxicity. I think it comes down to an individual assessment of the risks. If I told you that you have a 20% risk of your cancer coming back, versus your 70% chance of your cancer coming back and you are miserable on this therapy, all of a sudden 20% doesn’t look so bad.
He goes on to discuss various trials, including the ASSURE trial they conducted of which he says:
One thing that we did learn from this trial is that tolerance for the toxicity associated with targeted therapy in the adjuvant setting is not the same as in the metastatic setting. In this trial 41% of patients stopped therapy early, not because disease returned, or because they finished, but because of toxicity. I think it comes down to an individual assessment of the risks. If I told you that you have a 20% risk of your cancer coming back, versus your 70% chance of your cancer coming back and you are miserable on this therapy, all of a sudden 20% doesn’t look so bad.
My concern about this, because at the end of the day, if this trial matures and it is negative, will it be negative because the agents did not work, or because the patients could not tolerate the side effects. And too many patients stopped the trial early or had dose reductions. I’m afraid it is not going to be interpretable.
Aside from the theoretical reasons for supposing that none of these agents CAN be expected to work as adjuvants, this issue of interpretability may well sink all of these attempts. He goes on to observe that it's anybody's guess whether any of these trials and nay of these drugs will even have any relevance by the time the jury's finally in! All, we hope, will have been superseded by then by much more effective treatments.
Some time has elapsed since the work he was reporting on. From the recent AVEO tivozanib fiasco, we see, writ large, the non-feasability of carrying through these trials in the US. Recruitment problems are also at present looking almost insuperable in the UK. Meantime, there don't seem to be any preliminary findings of success from any of these trials, whether completed or still ongoing.
You will, I'm sure, readily appreciate many of these issues since you're encountering the problems at first hand and, as you'll read, you would be far from the first to drop out of a trial before completion, if you decide not to stay the course.
[On a purely personal note, I'm confident you'll forgive me if I pass a comment about your situation. In your shoes, I would be carefully weighing the hypothetical benefits of being in the trial against the compromise of my lifestyle. If you are on an agent which is immunosuppressive and which prejudices your daily activities via the unpleasant side-effects, you might be better off if you were feeling well and able to devote yourself, rather, to optimising your lifestyle - diet, regular exercise, meditation, etc? If the effects of the trial are undermining your general health care while holding out purely putative benefits, you might be better off not in it?]
As you are wont to say, 'I hope this helps'.
Live life. Do not obsess about your disease...it could be gone. Adjuvant theropy for RCC has not shown to increase life spans. And it decrease quality of life. Whack-a-mole seems to work better.
-
Thanks for the detailed responseTexas_wedge said:Could you name some? Or tell where the info came from?
Todd, perhaps I can save him the trouble. I've referred you to these materials before, summarised the outcome before and also explained the rationale for having low expectations of success, previously. This time I'll go further, detail a good source and quote some key excerpts.
The whole matter was given a good going over at the 2012 KCA National Patients Conference at MDAnderson in Texas. This topic was comprehensively covered by Chris Wood, by common consent the best onco-urological surgeon in the World. Peggy Zuckerman from California (who has paid a very occasional visit here, was one of the key participants on KIDNEY-ONC and now is on Smart Patients) performed a great service for us all in reproducing most of that Conference's proceedings, together with the slides at her excellent WordPress blog which you might care to explore. There's days/weeks of reading there so I'll point you to the part relevant for present purposes, viz:
http://peggyrcc.wordpress.com/2012/06/
Since there's a vast amount of material there, I'd recommend that you scroll to the bottom of that entry and then back up to find the first of Chris Wood's four talks: Locally Advanced RCC/Kidney Cancer; Dr. Chris Wood; Options & Treatment 1/4 Parts
You'll find a lot of good stuff there. I promised a few key quotes, so here goes:
Adjuvant Therapy means some form of therapy– chemo, radiation, vaccine, whatever–after complete surgical tumor resection with the idea to decrease the risk of recurrence of disease. The benefit is that the patient has already had surgery before getting additional therapy, but the downside is that many of those patients may have been cured by the surgery and they may get treatment they don’t really need.
That was the point I made to you when you were first contemplating entering the EVEREST trial. He goes on to present a very clear and intelligent analysis of this field. The use of all adjuvant treatments prior to the targeted therapies is dismissed easily:
Adjuvant Therapy: 2012
A variety of trials have been performed. Many patients have participated. They include radiation, embolization, energy ablation, a variety of different hormonal therapies, immunotherapies with interferon and interleukin 2, all having been used in an adjuvant setting. There have been a variety of vaccines preparations and we did a Phase III trial of thalidomide trial here. To date, not one of these therapies has shown benefit in the adjuvant setting. In fact, many of the patients on the treatment arms did worse than those who were not treated.
Then we get to the nub of your question
What about targeted therapies? That is also the great unknown where things stand with targeted therapies in the adjuvant setting.
Since 2006 there have been seven new agents against kidney cancer. It’s been a revolution. And to be honest, many have benefited from that advance. How do we use these agents in the context of adjuvant therapy?
There is a variety of trials recently completed or in accrual, ongoing. Tthe ARISER Trial used an antibody called G250 against Carbonic Anhydrase IX, and patients were randomized to get either antibody or placebo. This trial completed accrual many years ago, in fact, and we are still awaiting results which leads me to believe that is probably going to be a negative trial.
One thing that we did learn from this trial is that tolerance for the toxicity associated with targeted therapy in the adjuvant setting is not the same as in the metastatic setting. In this trial 41% of patients stopped therapy early, not because disease returned, or because they finished, but because of toxicity. I think it comes down to an individual assessment of the risks. If I told you that you have a 20% risk of your cancer coming back, versus your 70% chance of your cancer coming back and you are miserable on this therapy, all of a sudden 20% doesn’t look so bad.
He goes on to discuss various trials, including the ASSURE trial they conducted of which he says:
One thing that we did learn from this trial is that tolerance for the toxicity associated with targeted therapy in the adjuvant setting is not the same as in the metastatic setting. In this trial 41% of patients stopped therapy early, not because disease returned, or because they finished, but because of toxicity. I think it comes down to an individual assessment of the risks. If I told you that you have a 20% risk of your cancer coming back, versus your 70% chance of your cancer coming back and you are miserable on this therapy, all of a sudden 20% doesn’t look so bad.
My concern about this, because at the end of the day, if this trial matures and it is negative, will it be negative because the agents did not work, or because the patients could not tolerate the side effects. And too many patients stopped the trial early or had dose reductions. I’m afraid it is not going to be interpretable.
Aside from the theoretical reasons for supposing that none of these agents CAN be expected to work as adjuvants, this issue of interpretability may well sink all of these attempts. He goes on to observe that it's anybody's guess whether any of these trials and nay of these drugs will even have any relevance by the time the jury's finally in! All, we hope, will have been superseded by then by much more effective treatments.
Some time has elapsed since the work he was reporting on. From the recent AVEO tivozanib fiasco, we see, writ large, the non-feasability of carrying through these trials in the US. Recruitment problems are also at present looking almost insuperable in the UK. Meantime, there don't seem to be any preliminary findings of success from any of these trials, whether completed or still ongoing.
You will, I'm sure, readily appreciate many of these issues since you're encountering the problems at first hand and, as you'll read, you would be far from the first to drop out of a trial before completion, if you decide not to stay the course.
[On a purely personal note, I'm confident you'll forgive me if I pass a comment about your situation. In your shoes, I would be carefully weighing the hypothetical benefits of being in the trial against the compromise of my lifestyle. If you are on an agent which is immunosuppressive and which prejudices your daily activities via the unpleasant side-effects, you might be better off if you were feeling well and able to devote yourself, rather, to optimising your lifestyle - diet, regular exercise, meditation, etc? If the effects of the trial are undermining your general health care while holding out purely putative benefits, you might be better off not in it?]
As you are wont to say, 'I hope this helps'.
It's very much appreciated. I'm not sure the advice I received from my RCC specialists was in contradiction to anything you've presented. It appears it was not. It wasn't an easy decision to make and I'm still open to reason and evaluating what I'm doing and why.
Both of my RCC oncologists, Dr. Figlin and Dr. Pal, were primarily concerned about being able to stay on the drug for a full year of the study. They disagreed about which of the two drugs would be best for that (Dr. Figlin thought side effects were a non-issue for me given my generally good health, and for that reason I should go on the votrient study, while Dr. Pal thought Everolimus was much more likely to be tolerated in terms of side effects and for that reason he encouraged me to go on that trial). Dr. Figlin was neutral on particpating in a trial at all with regards to his advice to do a trial or not and left the decision completely up to me. If I did do one, he suggested the votrient one was the best choice. Dr. Pal thought I should try something given my high probability of recurrence (about 50%, both doctors agreed on this as did my uncle) and in his opinion the low likelihood that everolimus was going to cause me any problems. Patients in an adjuvant setting aren't as willing to tolerate side effects, but I also would guess that patients in adjuvant setting of a drug trial (where the effectiveness is unknown) are even less willing to tolerate side effects. This was the point the two doctors raised in our discussions.
If I'm having side effects, they are pretty mild and 4 months has been not too bad. I doubt I'll regret having tried it now that I have 4 months of it under my belt, but I suppose it could still happen.
It helps me better understand your reasoning.
Best wishes,
Todd
Discussion Boards
- All Discussion Boards
- 6 Cancer Survivors Network Information
- 6 Welcome to CSN
- 122.6K Cancer specific
- 2.8K Anal Cancer
- 456 Bladder Cancer
- 312 Bone Cancers
- 1.7K Brain Cancer
- 28.6K Breast Cancer
- 408 Childhood Cancers
- 28K Colorectal Cancer
- 4.6K Esophageal Cancer
- 1.2K Gynecological Cancers (other than ovarian and uterine)
- 13.1K Head and Neck Cancer
- 6.4K Kidney Cancer
- 681 Leukemia
- 803 Liver Cancer
- 4.2K Lung Cancer
- 5.1K Lymphoma (Hodgkin and Non-Hodgkin)
- 242 Multiple Myeloma
- 7.2K Ovarian Cancer
- 70 Pancreatic Cancer
- 493 Peritoneal Cancer
- 5.6K Prostate Cancer
- 1.2K Rare and Other Cancers
- 544 Sarcoma
- 743 Skin Cancer
- 659 Stomach Cancer
- 192 Testicular Cancer
- 1.5K Thyroid Cancer
- 5.9K Uterine/Endometrial Cancer
- 6.4K Lifestyle Discussion Boards