The Cancer Survivors Network (CSN) is a peer support community for cancer patients, survivors, caregivers, families, and friends! CSN is a safe place to connect with others who share your interests and experiences.
Gleason 7 Active Survellance
Yesterday I had a consult with a very good surgeon at the UNM Cancer Center. He does a lot of prostate removals with a high success rate and low side effects. He said because of my previous TURP and bladder opening scaring he would not recommend surgery, as it was sure to cause incontinence. He thought I should try active surveillance, which of course made me happy. I was diagnosed in Feb 18. I will still consult with MD Anderson on the Proton treatment, but this was very interesting so I thought I would share it. He did order an additional genetic test besides the Polaris and also a 3T MRI and Bone scan which MD Anderson has order for later in the month. I will try to get this done locally and share the results prior to going to Houston. My PSA is 13.67, Gleason 3 +4 in two cores at -15% one core 3+3 at-5%. He said that Active Surveillance should be safe with regular PSA test, but you never know. Although I am an intermediate risk, with Gleason score 7 because the percentage is -15% he said this is very similar to a Gleason 6. Although treatment may be needed in the future the older you get the better it will be since even radiation might cause substaintial QOL loss due to my preexisiting condition with the scaring. If anyone has been down this road or has advice please share. Thank you!
Comments
-
.
I am in year 10 of an active surveillance protocol
Depending on how extensive the 3+4=7's really are, there is a possibility that you may qualify for AS.
In my opinion PSA tests only will not do the job; you will need a biopsy directed by a t3 multiparametric MRI.
Here are some previous threads for you to read. Afterward reading through these threads, please get back to me at this thread so I an answer any of your questions or concerns
https://csn.cancer.org/node/315653
https://csn.cancer.org/node/315620
Here are some
-
AShopeful and optimistic said:.
I am in year 10 of an active surveillance protocol
Depending on how extensive the 3+4=7's really are, there is a possibility that you may qualify for AS.
In my opinion PSA tests only will not do the job; you will need a biopsy directed by a t3 multiparametric MRI.
Here are some previous threads for you to read. Afterward reading through these threads, please get back to me at this thread so I an answer any of your questions or concerns
https://csn.cancer.org/node/315653
https://csn.cancer.org/node/315620
Here are some
Thank you Hopeful and optimistic
-
Hello
i would Demand genomic testing ..I was diagnosed back in December 3 cores positive 3+3. 3+4. 3+4 7ml and 8 ml Tumors glesson 4 involvement 10% they said i was low end intermediate ..seen 8 drs and radiologist ..of course the last dr ordered genomic testing ..and now 5 months later test results saying the cancer is of high risk ..ctibiform pattern ..I shold treat soon could be worse now than back in dec..so now I’m rushed and scared as hell ...
-
Combination of a TURP and RP
SantaZia,
Just want to share my own experience which has one thing in common: We both had a TURP.
I was diagnosed with prostate Ca thru TURP samples that were sent to pathology. You did not mention how long ago was your TURP done. After my Turp I was diagnosed with 3+3, had TRUS biopsy 2.5 months later and was diagnosed with 4+3 (55/45) which led me to surgery 5 months later. Thankfuly, post op I was dow to 3+4 (60/40).
I recovered continence 98% by the end of 3 months post op which improves further to about 99% with still some stress incontinece on strenuous activity and sudden movents and twisting.
Recovery of erectile function is whole different story. I am 18 months post RP now and so far nothing spontaneous, no sign of feeling something is coming- really nothing. I did extensive and expensive penile rehab using Cialis, Viagra, VED, TRIMIX, BIMIX, L Arginine etc.
i lost 2+ inches of length and did not recover a bit of that. Orgasams are another disappointment, non existent. At time of RP I was 51.
Life sucks big after RP.
MK
-
Location of cancer?
Hi SantaZia,
One thing I would look into is the location of the cancer, is it close to the edge of the Prostate or buried deep down inside. The 3+4 is a little more agressive than the 3+3 and if the cancer is close to the edge of the Prostate then I would think treatment would be a little sooner than later. Don't want to let it escape the gland, then you in a whole nother ball game.
My surgery experience is a lot different than MK's. I had a Robotic RP and it took me about a year & a half to recover the ED thing and about the same for the urine leakage with improvement all along the way. I still wear a light daily pad to catch the ocasional dribble and if I move an odd way, but I am OK with that. if you want to choose radiation I like Proton. It's a fixed length beam that does not go past the target, so no exit tissue damage. Good choice in my opinion.
Dave 3+4
-
Asking
"because of my previous TURP and bladder opening scaring he would not recommend surgery, as it was sure to cause incontinence. "
Hey Santa Zia... if you consult with that surgeon again could you ask him about the mechanics behind his recommendation? That is, how does removal of prostate tissue in the urethra pathway, and scarring at the bladder neck result in prohibitions of future treatments? I am having trouble visualizing how the mechanics work during prostate removal that would be affected by the TURP and scarring.
It would be helpful if we could hear his answer... or if anybody else already has an idea how TURP and scarring interferes with RP... though I have asked this before on this forum.
-
AS or TreatmentMK1965 said:Combination of a TURP and RP
SantaZia,
Just want to share my own experience which has one thing in common: We both had a TURP.
I was diagnosed with prostate Ca thru TURP samples that were sent to pathology. You did not mention how long ago was your TURP done. After my Turp I was diagnosed with 3+3, had TRUS biopsy 2.5 months later and was diagnosed with 4+3 (55/45) which led me to surgery 5 months later. Thankfuly, post op I was dow to 3+4 (60/40).
I recovered continence 98% by the end of 3 months post op which improves further to about 99% with still some stress incontinece on strenuous activity and sudden movents and twisting.
Recovery of erectile function is whole different story. I am 18 months post RP now and so far nothing spontaneous, no sign of feeling something is coming- really nothing. I did extensive and expensive penile rehab using Cialis, Viagra, VED, TRIMIX, BIMIX, L Arginine etc.
i lost 2+ inches of length and did not recover a bit of that. Orgasams are another disappointment, non existent. At time of RP I was 51.
Life sucks big after RP.
MK
MK I have heard the surgery issues. I am sorry for yours. I have done intermittent cauterization since 2000. Okay I had a TURP in 2003. I probably didn't need it since it was confirmed that I had neurogenic bladder retention. It is a drag but a way of life. Surgery isn't an option for me as I have had a couple of bladder neck dilations already. This is where the bladder neck is stretched so you can continue cauterization. My PSA was low but not tested from 2012 to 2018 when it showed up as high 13.78 and 13.20. If I used the John Hopkins scale I would be high intermediate. However due to the long term cautheration 6 times a day two urologists believe that has raised my number. Thanks MK your comments help. I will continue consults with my surgeon who recommended AS on Tuesday. I also have a visit with the MD Anderson proton folks after that. My question for them is can they avoid the damaged bladder neck. Best to you.
-
AS or TreatmentClevelandguy said:Location of cancer?
Hi SantaZia,
One thing I would look into is the location of the cancer, is it close to the edge of the Prostate or buried deep down inside. The 3+4 is a little more agressive than the 3+3 and if the cancer is close to the edge of the Prostate then I would think treatment would be a little sooner than later. Don't want to let it escape the gland, then you in a whole nother ball game.
My surgery experience is a lot different than MK's. I had a Robotic RP and it took me about a year & a half to recover the ED thing and about the same for the urine leakage with improvement all along the way. I still wear a light daily pad to catch the ocasional dribble and if I move an odd way, but I am OK with that. if you want to choose radiation I like Proton. It's a fixed length beam that does not go past the target, so no exit tissue damage. Good choice in my opinion.
Dave 3+4
Hi Clevalandguy. I agree the location is important. It appears to be in the middle of my very small prostate gland. The prostate gland is relatively small, measures 3.1 cm cephalocaudal by 2.2 cm AP by 3.9 cm transversely for an estimated volume 14 mL. With diffusion-weighted imaging and ADC map a focal lesion within the mid gland extending to adjacent base and apex measures 1.8 cm largest transaxial plane. Lesion involves the peripheral zone of the mid gland anteriorly extending to adjacent apex and base and into the adjacent transition zone. This lesion shows significant diffusion restriction, fairly homogeneous T2 hypointensity and early suspicious contrast enhancement. There are no features of gross extraglandular spread and no involvement of seminal vesicles. I have some pre-existing issues with scaring on the bladder neck due to TURP and 6 times a day cauterization since 2000. I appreciate your comment. I will see if the MD Anderson proton folks can stop that beam just before hitting the bladder. If so, that will certainly increase my options. Best to you!
-
AS or Treatment
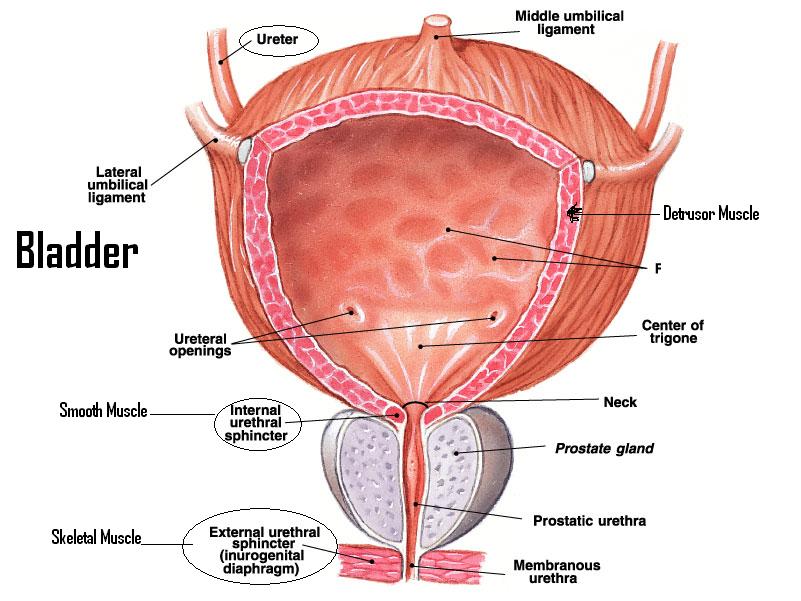
Thank you for the diagram I was actually wanting a nice clear one. I have the top surgeon in the state. High volume surgeries with a high level of success and highest certification in robitics. He is the one that recommended AS although that is what I wanted too. I meet with him next week and will ask. Here are his notes from my last visit Because of his chronic catheterizations, he has developed a recurrent bladder neck contracture and has had various dilating procedures performed by Dr. Anderson in the past and he actually underwent a transurethral resection of the prostate in 2003, which did not really resolve his urinary retention. We also went over the principle treatment options including active surveillance, radical prostatectomy and radiation therapies. We talked about pros and cons of all these treatments. He clearly seems to be in good health and, based on his family history and his medical history, I think he has at least a 10-year life expectancy and he seems to have a favorable intermediate risk prostate cancer and, ordinarily, I think any treatment option would be reasonable but, in his particular situation, I think his history is very complicating. I told him that should he choose a radical prostatectomy I am concerned that his risk of incontinence would be higher and his risk of scarring could be higher, which could cause him chronic complications. With respect to radiation therapy I think there is also risks that his bladder neck contracture is worsened and, of course, his catheterization could be a complicating factor for that as well. We also talked about just general controversies with prostate cancer and the fact that low volume Gleason 7 disease is, by NCCN guidelines, okay for surveillance in some situations. I told him that his higher than normal PSA; however, is a concern. So I am certainly on the edge. Everyone's input has been exceptional. Not too many folks have enough experience or knowledge to discuss this with me, so I very much appreciate what everyone is saying. Thank you!
-
fascinating
That was fascinating... to hear the doctor 's own words.
I still have unpleasant memories of catheterization... I'm surprised it didn't do more damage to my urethra and bladder than was done as I could feel it irritate everything, especially when it would get infected. But at the time I didnt have a choice.
I have to give you props... your attitude is surprisingly upbeat considering the tough circumstances.
-
Good pictureGrinder said:Asking
"because of my previous TURP and bladder opening scaring he would not recommend surgery, as it was sure to cause incontinence. "
Hey Santa Zia... if you consult with that surgeon again could you ask him about the mechanics behind his recommendation? That is, how does removal of prostate tissue in the urethra pathway, and scarring at the bladder neck result in prohibitions of future treatments? I am having trouble visualizing how the mechanics work during prostate removal that would be affected by the TURP and scarring.
It would be helpful if we could hear his answer... or if anybody else already has an idea how TURP and scarring interferes with RP... though I have asked this before on this forum.
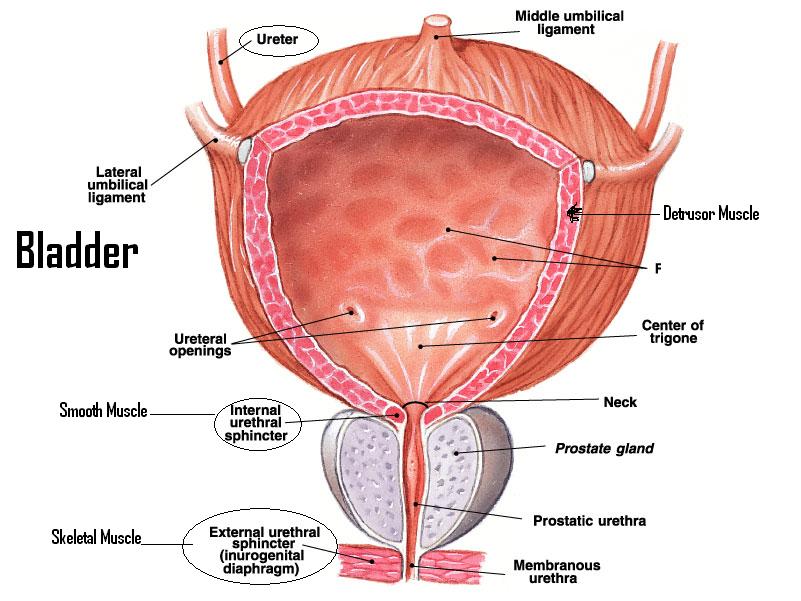
I printed this off. The inside of my bladder looked a lot whiter verses the illustration during my cystoscopy. Those dimples on your picture looked like white covered domes. And when I flexed my kegels they looked like balloons. Anyway, thanks for posting the picture.
-
Scarring on the Bladder NeckGrinder said:Asking
"because of my previous TURP and bladder opening scaring he would not recommend surgery, as it was sure to cause incontinence. "
Hey Santa Zia... if you consult with that surgeon again could you ask him about the mechanics behind his recommendation? That is, how does removal of prostate tissue in the urethra pathway, and scarring at the bladder neck result in prohibitions of future treatments? I am having trouble visualizing how the mechanics work during prostate removal that would be affected by the TURP and scarring.
It would be helpful if we could hear his answer... or if anybody else already has an idea how TURP and scarring interferes with RP... though I have asked this before on this forum.
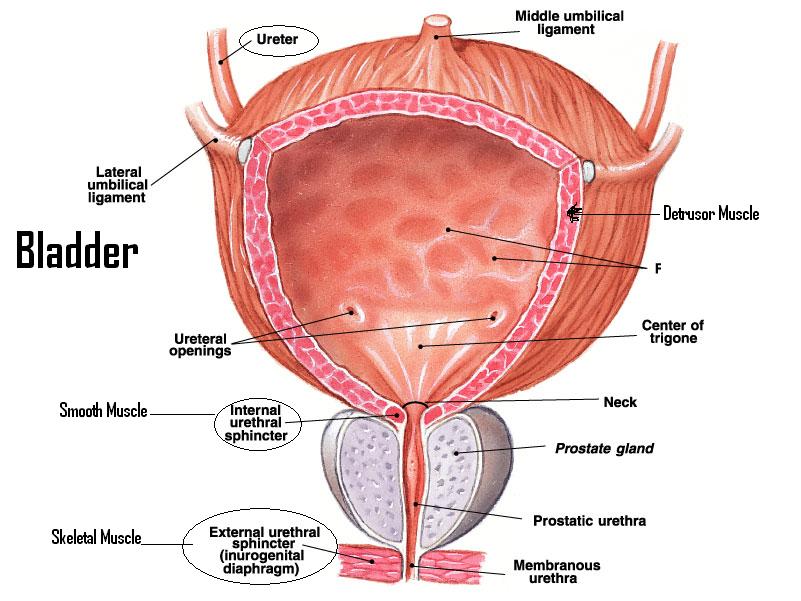
Grinder to be more specific my issue is a stricture within the membranous urethra membranous urethra, which includes a muscle called the external urinary sphincter surrounding the bladder neck.
-
-
Hi neilm, sorry you are dealing with this. Of course, everyone wants AS, I sure did. However after two genetic tests and a T3 MRI I was convinced that I need treatment. I consulted with University Hospitals MD Anderson and UNM Cancer as well as other consultants. Most were covered by Medicare. I also had my biospy review at John Hopkins. It turned out different that MD Anderson's review. I went with the traditional 42 treatments with Radiation and 6 months on Lupron. I also had the SpaceOar injection to protect my colon and nerves. It was successful. I would suggest you get all the testing and consults you can. If the PC excapes to the bone and other organs you have 5-7 years usually with hormone treatment and ending with Chemo. I had a friend who had advanced PC and really couldn't stop it although he did have his prostate removed it was too late. Do your research. University Cancer Centers have stats and data that others don't keep. Best wishes, Andy
-
Thanks SantaZia, Your comments are well taken. I would like the easy way out here, it would almost be easier if my oncologist had not suggested AS as a pathway. I am working with an NCCN University. I think I need more information , perhaps a second genetic test , and possibly a PSMA Pet scan although not sure if that helps.
Discussion Boards
- All Discussion Boards
- 6 Cancer Survivors Network Information
- 6 Welcome to CSN
- 122.6K Cancer specific
- 2.8K Anal Cancer
- 457 Bladder Cancer
- 312 Bone Cancers
- 1.7K Brain Cancer
- 28.6K Breast Cancer
- 407 Childhood Cancers
- 28K Colorectal Cancer
- 4.6K Esophageal Cancer
- 1.2K Gynecological Cancers (other than ovarian and uterine)
- 13.1K Head and Neck Cancer
- 6.4K Kidney Cancer
- 683 Leukemia
- 804 Liver Cancer
- 4.2K Lung Cancer
- 5.1K Lymphoma (Hodgkin and Non-Hodgkin)
- 242 Multiple Myeloma
- 7.2K Ovarian Cancer
- 70 Pancreatic Cancer
- 493 Peritoneal Cancer
- 5.6K Prostate Cancer
- 1.2K Rare and Other Cancers
- 544 Sarcoma
- 744 Skin Cancer
- 661 Stomach Cancer
- 193 Testicular Cancer
- 1.5K Thyroid Cancer
- 5.9K Uterine/Endometrial Cancer
- 6.4K Lifestyle Discussion Boards

