Small cell esophageal cancer

Hello friends, this post is on the behalf of my father.
He was recently diagnosed with small cell esophageal cancer(apparently a very aggressive form). We are still in the early stages where we're trying to figure out what the hell is going on. He is very young at 45 years old and has had reflux issues for a very long time. For the last month or so he has been complaining of pain in the general esophageal area. He is otherwise very very healthy. His blood tests came back negative for anemia and he has lost very little weight (which could be due to the fact that he and my mother have been dieting). He feels strong and the pain is mostly centralized. I'm not entirely sure what I'm looking for here other than general advice and reassurance. The "small cell" bit of it has given me very scary internet results and a bleak point of view. It also makes me believe it has spread despite my dad feeling otherwise 100% (we don't have information on how far it has spread yet). Our current care provider is Kaiser Permanente in Southern California. All the information I have just listed is all the information we have thus far. The surgeon apparently, in front of my parents, pulled out his phone to search up information on small cell esophageal cancer due to the rarity of it -- which I find to be anything but reassuring and makes me feel like my dad isn't in very good hands. I'm researching alternative centers and doctors to get that second opinion and the best course of treatment.
As of right now, more scans are scheduled (specifically to see if it had spread anywhere else) to determine when surgery should happen. The game plan currently is surgery first, then chemo/radation.
Does anyone have any insight? I'm doing everything I can to keep my dad around, he is so young. I am set to graduate college (the first in my family) May 2018 and at the very least I need him to be there. Anything helps. Thank you.
Comments
-
*insight not incite
*insight not incite
0 -
Hello
Hello yasminvarg,
I'm not familiar with small cell EC, so I googled it. You're right, it's quite rare. Sorry if I can't offer much in the way of specifics, but I can offer some generalities. Getting your father to a good hospital with good doctors is the most important thing you can do that is in your control. If you feel like you're not in good hands, by all means seek out a top flight cancer center that may have some experience dealing with scec. You may have a hard time finding folks who are experts, due to the rarity, but you can hopefully find somewhere that is more than one google search ahead of you in knowledge. Also, especially due to the rarity, I would seek out a second opinion, even if you love Kaiser Permanente. A large number of initial diagnoses are either wholly or partially changed with a second opinion. Also, a second opinion may offer different options for treatment that you may prefer.
45 is very young for this stuff, but youth is a strong ally in this fight. That your father is young, strong and otherwise healthy will help him greatly in his fight. Unfortunately, EC has a bad habit of hitting relatively young people more than other cancers do. I don't know the standard teatment for scec, but for adenocarcinoma and squamous cell carcinoma (the 2 most common forms of EC) the desired standard treatment (if the person is healthy enough and the cancer is caught early enough) is chemo/radiation, then surgery. I don't know what the benefit of reversing that order is, but I don't know anything about scec, either.
Sorry I have so little to offer.
Wishing you guys the best,
Ed
0 -
Thank you so much
Thanks a million for the well thought out response. I live away from home but I have called my mom and relayed this information to her. She will be collecting all of his medical records and scans and pushing for a special referral for a second opinion. I’m glad you mentioned UCI as that was one of our initial alternatives to Kaiser. Again, thank you very much.
0 -
"Yasminvarg"~Some info 4 SCEC+a 2nd surgeon 2C +prayersDeathorglory said:Hello
Hello yasminvarg,
I'm not familiar with small cell EC, so I googled it. You're right, it's quite rare. Sorry if I can't offer much in the way of specifics, but I can offer some generalities. Getting your father to a good hospital with good doctors is the most important thing you can do that is in your control. If you feel like you're not in good hands, by all means seek out a top flight cancer center that may have some experience dealing with scec. You may have a hard time finding folks who are experts, due to the rarity, but you can hopefully find somewhere that is more than one google search ahead of you in knowledge. Also, especially due to the rarity, I would seek out a second opinion, even if you love Kaiser Permanente. A large number of initial diagnoses are either wholly or partially changed with a second opinion. Also, a second opinion may offer different options for treatment that you may prefer.
45 is very young for this stuff, but youth is a strong ally in this fight. That your father is young, strong and otherwise healthy will help him greatly in his fight. Unfortunately, EC has a bad habit of hitting relatively young people more than other cancers do. I don't know the standard teatment for scec, but for adenocarcinoma and squamous cell carcinoma (the 2 most common forms of EC) the desired standard treatment (if the person is healthy enough and the cancer is caught early enough) is chemo/radiation, then surgery. I don't know what the benefit of reversing that order is, but I don't know anything about scec, either.
Sorry I have so little to offer.
Wishing you guys the best,
Ed
Hello
It goes without saying that we are sorry that your dad has now been diagnosed with Esophageal Cancer. Hopefully "Kaiser" will give you permission to have a SECOND opinion, and hopefully it will NOT have to just be in their NETWORK. If so, that limits your choices, but you will have to go with what you have. By your letter, I'm not certain that the doctor exuded a lot of confidence if he had to research it more before giving you an answer. Naturally, there will be lots of tests that will have to be performed.
For Adenocarcinoma @ the GE junction, & Squamous Cell Esophageal cancers, the usual modus operandi is chemo/radiation first (neoadjuvant) then Esophagectomy afterwards. Radiation is aimed specifically at the tumor itself, while the chemo circulates throughout the entire body. However, I must tell you that all my research relative to Esophageal cancer has revolved around the two main types listed above. This is the first time I have read a post that gave “Small Cell Esophageal Cancer” as the diagnosis. And I have to tell you that all the references I have listed below do not hold as much promise for a successful solution as do the 2 main types. This is indeed a rare cancer—the doctor was correct about that. Now how much experience he has with it is another matter. The fact that the doctor consulted his “smart phone” to give you more information wasn’t much of a confidence builder I am sure.
 According to the reports that I’ve read in references below are “all over the map” when it comes to the correct order in which to proceed to try to find the best possible outcome for each individual patient. It seems that some say surgery can be a part of the treatment, while others say only chemotherapy and/or radiation.
According to the reports that I’ve read in references below are “all over the map” when it comes to the correct order in which to proceed to try to find the best possible outcome for each individual patient. It seems that some say surgery can be a part of the treatment, while others say only chemotherapy and/or radiation. So for that reason, I do not feel qualified to give you a definitive explanation of what tests should be accomplished or how the stages are determined.
 I wish I could. I am very familiar with Adenocarcinoma @ the Gastroesophageal junction because that was the diagnosis of my husband. But in your case, I can only express my sorrow at knowing that the prognosis for Small Cell Esophagus Cancer is not as good as it is for the two most prevalent types. The most successful treatment has been tri-modal for the two main types—preferably pre-op chemo/radiation and then surgery. But this SCEC doesn’t necessarily follow that regimen. You should definitely, ask for copies of all the tests, and scan results when your dad is tested. Another medical facility will want to see all of them, and review them along with conducting many of their own exams.
I wish I could. I am very familiar with Adenocarcinoma @ the Gastroesophageal junction because that was the diagnosis of my husband. But in your case, I can only express my sorrow at knowing that the prognosis for Small Cell Esophagus Cancer is not as good as it is for the two most prevalent types. The most successful treatment has been tri-modal for the two main types—preferably pre-op chemo/radiation and then surgery. But this SCEC doesn’t necessarily follow that regimen. You should definitely, ask for copies of all the tests, and scan results when your dad is tested. Another medical facility will want to see all of them, and review them along with conducting many of their own exams. Mayo Clinic just released a study in April of this year that indicated that only 12% of first opinions were CORRECT, out of all the patients that had come to them for a 2nd opinion in the last year and more. Pittsburgh, PA is a far cry from California, so I trust you can find a competent thoracic surgeon on the West Coast that is totally familiar with Minimally Invasive Procedures if surgery is part of the treatment regimen for your dad. There is one terrific thoracic surgeon, Dr. Ninh Nguyen, who operates out of UCIrvine in California. If your dad’s insurance will allow a SECOND opinion, I would certainly consult with Dr. Nguyen. He worked with Dr. James D. Luketich when the Ivor Lewis Minimally Invasive Esophagectomy was first being introduced at UPMC. He has written numerous articles that have been accepted by medical journals for publication. I always like to know how many medical articles a doctor has written. This gives me an idea of his understanding of this cancer.
Dr. Ninh Nguyen, Chief, Division of Gastrointestinal Surgery, UC Irvine School of Medicine
Division of Gastrointestinal Surgery: http://www.surgery.uci.edu/gastrointe...
And if I may offer just a note about an “EDITING FEATURE” here, it will be helpful to you when posting future responses. We all sometimes use the wrong word, or misspell something. So any time you are the one posting the original article, you will have an EDIT button. Look for it. It will either be at the top of your letter or at the bottom. When you CLICK ON THAT BUTTON, it will bring up your entire post. At that point you are in an "edit mode" and can change, add or delete anything you wish. And so I thought as a "newbie", I would help you out. So even "after" it is posted on the board, you can always go back and "edit" it, if you see something you want to change, rather than posting a new letter just to change a word. When you've made the necessary change or changes, simply click on the SUBMIT button, and the revised edition will post. I findfirst composing my letters in the WORD format and then pasting them works well for me.
Forgive me for not being able to be more helpful, but this is the best I can do for you.
 Both "ED" and I are very familiar with cancer terminology relating to Esophageal cancer usually, but in this case I feel totally inadequate to help you. As I read the articles, I could not get a clear idea of just what treatment protocols were considered “best” for this type of cancer. But know that there are many who read this site, and I know many pray for the people they correspond with here. It is my prayer that you will be able to find a competent Thoracic surgeon who is very familiar with Small Cell Esophageal Cancer, and that will know the very best way to treat your dad.
Both "ED" and I are very familiar with cancer terminology relating to Esophageal cancer usually, but in this case I feel totally inadequate to help you. As I read the articles, I could not get a clear idea of just what treatment protocols were considered “best” for this type of cancer. But know that there are many who read this site, and I know many pray for the people they correspond with here. It is my prayer that you will be able to find a competent Thoracic surgeon who is very familiar with Small Cell Esophageal Cancer, and that will know the very best way to treat your dad.Prayers for you and your dad,
Loretta Marshall
Wife of William, who was diagnosed with "Adenocarcinoma @ the Gastroesophageal Junction (GE) (T3N1M0) in 2002. If you read my "about me" page, you will know more about his treatment at the University of Pittsburgh Medical Center by Dr. James D. Luketich. ____________________________________________________________________
1. http://www.gomn.com/news/mayo-clinic-says-get-a-second-opinion-first-ones-are-frequently-wrong/
“MAYO CLINIC SAYS GET A SECOND OPINION – FIRST ONES ARE FREQUENTLY WRONG
By Melissa Turtinen - April 4, 2017 12:17 pm
The Mayo Clinic in Rochester did a study (published in a medical journal Tuesday) and found as many as 88 percent of patients who came to the clinic for a second opinion for a complex condition left with a new or more refined diagnosis, a news release says.
The Mayo Clinic says a different or more detailed diagnosis can change someone’s care plan “and potentially their lives.”
The study looked at 286 patients who were referred from primary care providers to Mayo Clinic’s General Internal Medicine Division in Rochester between Jan. 1, 2009, and Dec. 31, 2010. Here’s how the types of diagnostic errors breaks down:
- Only 12 percent of patients left the Mayo Clinic with the same diagnosis.
- In 21 percent of cases, the diagnosis was changed completely.
- In 66 percent of patients, their diagnosis was refined or redefined.
“Effective and efficient treatment depends on the right diagnosis,” Dr. James Naessens said in the release. “Knowing that more than 1 out of every 5 referral patients may be completely [and] incorrectly diagnosed is troubling – not only because of the safety risks for these patients prior to correct diagnosis, but also because of the patients we assume are not being referred at all.”
A lot of people don’t consider getting a second opinion because they either don’t know that’s something you can do, or because it can be expensive for people to see another doctor who may not be in their health insurance’s network, the Mayo Clinic says.
“Total diagnostic costs for cases resulting in a different final diagnosis were significantly higher than those for confirmed or refined diagnoses, but the alternative could be deadly,” Naessens said.
HOW TO ASK FOR A SECOND OPINION
It may seem a little awkward to ask your doctor for a referral to get a second opinion, but don’t worry – asking for a second opinion is pretty normal, U.S. News and World Report says, noting any doctor who is good at what they do will welcome a second opinion.
Here are some tips about seeking a second opinion:
– Don’t worry about asking for a second opinion for the minor things. Instead, seek a second opinion for serious or chronic issues, especially if you’re unsure about your doctor’s diagnosis or if the treatment for the issue is experimental or risky, U.S. News and World Report notes. But it’s important not to wait too long to get a second opinion, because you don’t want to delay treatment for too long, the Patient Advocate Foundation says.
– When asking for the second opinion, tell your doctor you just want to be fully informed about your diagnosis, prognosis and treatment, Compass Healthcare Solutions suggests. You can ask your doctor for a referral to see a specific doctor you have in mind, but WebMD says don’t see a doctor that is affiliated with your initial doctor – they probably won’t contradict them.
– Before you go see the new doctor, make sure you get a copy of your medical records and test results, the Patient Advocate Foundation says. Sometimes tests can be wrong, though so WebMD says you can ask for a second medical opinion and for the lab or pathologist to do the tests again.
– When you go in for your second opinion, remember you’re looking to confirm your current diagnosis – the second opinion isn’t always right, U.S. News and World Report says. Doctors may differ on your diagnosis or a treatment plan, and ultimately it’s your choice to decide what’s best for you, the Patient Advocate Foundation says.
For more information on when and how to get a second opinion, click here."
___________________________________________
2.
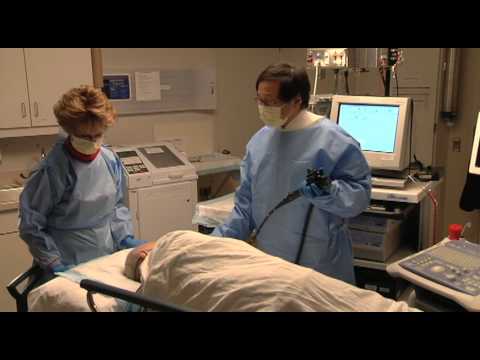
 https://www.youtube.com/watch?v=KnjQEe8qtjw
https://www.youtube.com/watch?v=KnjQEe8qtjw[My note: This is a 22-minute video, but it is not accompanied by any explanation of what is taking place. My reason for including this video is to let you see what an endoscopy of the Esophagus looks like. This is the clearest, and I might add, hard to watch video because it shows so much cancer inside the Esophagus. One can easily understand why people have swallowing difficulties. Now this is not to say that this is exactly what your father’s esophagus looks like inside, but it is just to show the extent of blockage that can be found when one is diagnosed with Esophageal Cancer.]
“ENDOSCOPY OF ESOPHAGEAL CANCER AND ACHALASIA
Dr.Julio Murra Saca Endoscopia El Salvador - Published on Aug 27, 2013
“Achalasia is an uncommon swallowing disorder that affects about 1 in every 100,000 people. The major symptom of achalasia is usually difficulty with swallowing. Most people are diagnosed between the ages of 25 and 60 years. Although the condition cannot be cured, the symptoms can usually be controlled with treatment. .. Achalasia is a chronic esophageal motility disorder associated with esophageal retention of foods and fluids, bacterial overgrowth, and impaired clearance of regurgitated gastric contents. These factors usually lead to chronic inflammation of the esophageal mucosa, which potentially increases the risk of hyperplasia, dysplasia, and esophageal cancer.”
_______________________________________________________________
3.
 https://www.youtube.com/watch?v=bp7cP05S_-g
https://www.youtube.com/watch?v=bp7cP05S_-gSymptoms and Treatment of Esophageal Cancer
Med Sym Tv - Published on Dec 27, 2016 - __
(4.56minute video)
______________________________________________________________________
4.
 https://www.youtube.com/watch?v=pIVWNjIOmd4
https://www.youtube.com/watch?v=pIVWNjIOmd4 Esophagus Cancer (adenocarcinoma)-Mayo Clinic
“Mayo Clinic - Published on Apr 22, 2010 – 4:00 minute video
Over time, Gastroesophageal Reflux Disease, or GERD, can lead to Barrett’s esophagus, dysplasia or even esophagus cancer (adenocarcinoma.) This video shows how cancer may gradually invade the esophagus, other organs and lymph nodes, progressing from early-stage disease to locally advanced disease to late-stage disease. It also discusses tests to locate cancer in the body, including a CT scan, PET scan, PET/CT scan and endoscopic ultrasound, and methods of treating cancer. Mayo Clinic has a very large team with an international reputation for its skill in diagnosing and treating reflux, Barrett’s esophagus and esophagus cancer. For more information, go to the Mayo Clinic website, http://www.mayoclinic.org/barretts-es...”
_________________________________________________________________________________________________
5. http://www.chsjournal.org/archive/vol37-no1-2011/case-report/primary-small-cell-carcinoma-of-the-esophagus-clinico-pathological-features-and-therapeutic-options
[My note: This has many references that went into preparing this abstract. While I don’t usually include all the authors under the printed abstract, in this case, I will include them because so many of the statements written in this abstract are followed by one or more numerical references. If you were to click on anyone of the authors below the main abstract, you would find exactly what that particular article had to say about this small cell carcinoma of the Esophagus.]
“Printed Edition ISSN: 2067 - 0656 , Electronic edition ISSN: 2069 - 4032 Volume 43 Issue 2 2017 April - June (quarterly)
Home Archive Vol.37, No.1, 2011 Case Report Primary Small Cell Carcinoma of the Esophagus: Clinico- pathological Features and Therapeutic Options
PRIMARY SMALL CELL CARCINOMA OF THE ESOPHAGUS: CLINICO- PATHOLOGICAL FEATURES AND THERAPEUTIC OPTIONS
ANDREA NEVÁREZ(1), A. SAFTOIU(2), M.S. BHUTANI(3)
(1)Gastroenterology Unit, La Fe Hospital, Valencia, Spain; (2)Research Center of Gastroenterology and Hepatology Craiova, University of Medicine and Pharmacy Craiova, România; (3) Department of Gastroenterology,Hepatology and Nutrition, UT MD Anderson Cancer Center, Houston,Texas,USA
Abstract: Primary esophageal small cell carcinoma (SmCC) is a rare disease with a poor prognosis despite agressive multimodality combination treatment.
This article presents the case of a 76-year old women diagnosed with pimary esophageal SmCC. The diagnosis was established by upper gastrointestinal endoscopy with biopsies that confirmed an esophageal SmCC positive to synaptophysin, chromogranin, CD56, TTF-1, and cytokeratin 8/18. Further staging procedures included CT, PET and EUS, followed by combination chemotherapy and radiotherapy. Restaging was then performed, again with PET and CT of the thorax, abdomen and pelvis. This was then followed by salvage esophagectomy due to the presence of residual tumor. Surgical pathology confirmed a 3 cm SmCC, with invasion of the submucosa and lymphovascular invasion. In conclusion, the article describes the rare occurrence of esophageal SmCC, together with the algorithm of diagnosis and staging based on state-of-the-art imaging methods. This was followed by combination chemoradiotherapy and surgical esophagectomy as the standard of care in this aggressive disease.
Keywords: esophageal small cell carcinoma (SmCC), positron emission tomography (PET), computer tomography (CT), endoscopic ultrasound (EUS)
Introduction
Esophageal small cell carcinoma (SmCC) is a very uncommon disease. It accounts for up to 0.4 to 2.8% of all esophageal carcinomas1. The disease has been managed with various forms of treatment that include surgical resection, radiotherapy, chemotherapy and combinations of them; nonetheless, even with the use of aggressive treatment the prognosis of the tumor is still poor. We present a case of a 76-year-old woman with diagnosis of primary esophageal SmCC.Case report
A 76-year-old woman with a three month history of sore throat and odynophagia associated with gastroesophageal reflux disease underwent an upper gastrointestinal endoscopy revealing a circumferential fungating mass, occupying 50% of the lumen, in the mid esophagus. She has no personal history of smoking or drinking alcohol. Tumor markers were within normal limits, with CEA levels of 1.9 NG/ML. The biopsy specimens showed SmCC positive to synaptophysin, chromogranin, CD56, TTF-1, and cytokeratin 8/18.
A positron emission tomography (PET) scan revealed hypermetabolic activity in the primary tumor, 4 cm beneath the carina, measuring 3 x 2 x 1 cm, with standardized uptake value (SUV) up to 3.8. No flourodeoxyglucose (FDG) avid lymphadenopathy was noted.
A thoracic and abdominal computer tomography (CT) scan showed no presence of lymph nodes or mediastinal lesions suspicious of metastasis.
Endoscopic ultrasound (EUS) showed no lymphadenopathy but penetration through the muscularis propria into the adventitia with tumor stage as uT3N0.
Chemotherapy was begun combined with radiotherapy as definitive therapy.
She completed a total of 5 cycles of chemotherapy consistent of cisplatin, etoposide and carboplatin.
She also received 50 Gy radiation therapy.
After this treatment she underwent restaging testing. Repeat EGD revealed persistence of the esophageal mass at 29 to 32 cm, occupying 40% of the circumference (Figure 1). Biopsy specimens continued to show small cell carcinoma.
Repeat PET scan showed a focal circumferential thickening of the wall of the esophagus in the middle third that had a low grade increased 18-FDG uptake suspicious of residual malignancy (SUV values of 4.6) (Figure 2).
There were no FDG avid lymphnodes in the neck, thorax, abdomen or pelvis. Her CT scan of thorax, abdomen and pelvis showed no evidence of distant metastatic disease. She was treated with salvage esophagectomy due to presence of the residual tumor. Surgical pathology revealed 3 cm small cell carcinoma with 95% viable tumor invading the submucosa without involvement of the muscularis propria. Lymphovascular invasion was identified.
Figure 1: Endoscopic image of a mass in the esophagus with central depression biopsies of which showed small cell cancer of the esophagus despite treatment with chemotherapy and radiation.
Figure 2: Fused CT-PET image showing an FDG avid lesion in the esophagus (blue arrowheads) corresponding with small cell cancer of the esophagus seen in figure 1.
Discussion
SmCC occurs as a primary tumor mainly in the lung and accounts for 16% of lung cancers2.
Extrapulmonary SmCC are rare, but many sites have been described including salivary glands, larynx, pharynx, prostate, bladder, endometrium, and gastro intestinal tract3-5.
Primary esophageal SmCC was first described in 1952 by McKeown6 and it is the most common location in the gastrointestinal tract. Esophageal SmCC is a very uncommon disease. It accounts for up to 0.4 to 2.8% of all esophageal carcinomas1.
Its clinical presentation is similar to other esophageal tumors. The most common symptoms are dysphagia, anorexia, weight loss, reflux and chest pain1, 7-10.
There have been some reports of paraneoplasic syndrome with ectopic secretion of hormones, but this is a rare finding1. The lesion is more frequently located in the mid – lower esophagus3, 7, 9, 10, 12.
Upper esophageal localization has been seen in approximately 5% of cases12.
No predisposing risk factor has been identified with SmCC, but some associations with smoking, alcohol consumption and Barrett’s disease have been made9, 12-14. The mean age of diagnosis is between 40 to 70 years, with male predominance.
When the disease is suspected confirmation by histological diagnosis has to be done with adequate staging. The prognosis of the tumor is poor, with median survival ranging from 7- 19 months3, 8-10,15. Most of the tumors have lymph node involvement and a high percentage of cases are diagnosed with distant metastasis (31-90%1); the most common site of metastasis is the liver, followed by peritoneum and bones1, 13.
Diagnosis is established by histological criteria for pulmonary small cell carcinoma proposed by the World Health Organization. It consists of small, round, ovoid or spindle-shaped cells with scanty cytoplasm, finely granular nuclear chromatin, and absence or not easily seen nucleoli 1, 3, 5. There can also be components of squamous cell carcinoma or adenocarcinoma in some tumors7, 10, 12, 16. Most common immunohistochemical neuroendocrine markers are neuron-specific enolase, chromogranin, synaptophysin and CD561, 3, 11, 17. Another marker that has been studied in lung tumors is thyroid transcription factor-1 (TTF-1), is almost always negative in gastrointestinal SmCC1. However in a study published by Yun PJ et al3; 71.4% TTF-1 positive tumors were reported, suggesting that it was a suitable marker for diagnosis and differentiation of esophageal SmCC. Esophageal SmCC is thought to originate from multipotential stem cells as initially proposed by Ho et al in 198418. These cells may differentiate into squamous, glandular or neuroendocrine cells, which may explain the coexistence of mixed tumors in up to 40-50% of cases of SmCC1.
Treatment protocols have not been established nor have been studied by prospective randomized trials, due to the low incidence rate of this disease. The reported cases of SmCC have been managed with various forms of treatment that include surgical resection, radiotherapy, chemotherapy and combinations of them. However prognosis is still poor even with the use of aggressive treatment because of the frequent presence of metastasis at time of diagnosis.
For limited disease (LD); defined as disease confined to the esophagus and adjacent organs with or without regional lymph node involvement1, 8, 9, 15, the most effective treatment has not been established. Many reports have combined surgery with chemotherapy and/or radiotherapy, with different survival rates.
In general the median survival rates in these patients with LD is between 8 to 24 months8, 9, 12, 15.
In a review published by Casas et al12, a significant survival difference was seen between limited and disseminated disease, as did also the size of tumor less than 5 cm and the use of combination therapy.
This has also been reported by Lv et al15 in clinical experience of 126 patients. It was seen that the stage of the disease and treatment with chemotherapy were independent prognostic factors for survival. They recommended the use of chemotherapy for the treatment of LD. Hudson et al8 reported that chemotherapy combined with radiation may provide an effective treatment for local control, avoiding the morbidity of extensive surgery.
It also recommended that surgery can be done in clinically selected patients where it may be reserved as salvage after documented local failure following chemoradiation, as done in our case. Ku et al9 has also reported that long term survival can be achieved without surgery when chemotherapy followed by chemotherapy with radiotherapy is used.
Nemoto et al19 reviewed 12 patients with LD that underwent surgery, and later were treated with radiation (some of them also treated with chemotherapy). They couldn´t determine the optimal local treatment due to the small number of patients, but their long-term survivors were treated with radiation and chemotherapy after surgery.
With these findings they got to the conclusion that good local control rates can be obtained by definite or postoperative radiation therapy, with concurrent chemotherapy.
Other studies also have shown that longest survivors have been seen in patients treated with esophagogectomy combined with chemotherapy or radiotherapy1, 9.
Nevertheless there have been reports where the response to chemotherapy is only 50%1. This could be explained by the number of tumors with mixed histology, and this can be handled by individualization of chemotherapy treatment.
Extensive disease (ED) is always treated with chemotherapy in those patients who have reasonable performance status. Median survival rates in this kind of patients ranges from 3 to 11 months9, 12, 15, 17, it is well known that extent of the disease has a strong impact in survival 1, 12, 13, 15, 20.
Chemotherapeutic agents are those similarly used for the treatment of lung small cell carcinoma. Most commonly used agents are cisplatine, etoposide, cyclophosphamide and doxorubicin; these agents are usually used in combination1. It is also important to say that because of the significant number of tumors that have mixed histology, individualization of chemotherapy should also be assessed. Radiation therapy may be also beneficial to patients who need palliative treatment in ED.
References
1. Brenner B, Tang L, Shia J, Klimstra D, Kelsen D. Small cell carcinomas of the gastrointestinal tract: clinopathological features and treatment approach. Semin Oncol 2007; 34: 43-50.
2. NCCN Practice Guidelines in Oncology. Small Cell Lung Cancer. 2010.
3. Yun JP, Zhang MF, Hou JH, Tian QH, Fu J, Liang XM, Wu QL, Rong TH. Primary small cell carcinoma of the esophagus: clinicopathological and inmunohistochemecal features of 21 cases. BMC Cancer 2007, 7:38.
4. O'Kane AM, O'Donnell ME, Shah R, Carey DP, Lee J. Small cell carcinoma of the appendix. World J Surg Oncol. 2008 Jan 15; 6: 4.
5. Zhu W, Jian-Yang M, Jun-Jie Y, Yong-Fan Z, Shang-Fu Z. Primary small cell carcinoma of esophagus: Report of 9 cases and review of literature. World J Gastroenterol 2004;10(24):3680-3682.
6. McKeown F. Oat cell carcinoma of the esophagus. J Path Bact 1952;64: 889–91.
7. Sun K, He J, Cheng G, Chai L. Management of primary small cell carcinoma of the esophagus. Chin Med J 2007;120(5):355-358.
8. Hudson E, Powell J, Mukherjee S, Crosby TDL, Brewster AE, Maughan TS, Bailey H, Lesser JF. Small cell oesophageal carcinoma: an institutional experience and review of the literature. Br J Cancer 2007; 96: 708- 711.
9. Ku GY, Minsky BD, Rusch VW, Bains M, Kelsen DP, Ilson DH. Small-cell carcinoma of the esophagus and gastroesophageal junction: review of the Memorial Sloan-Kettering experience. Ann Oncol 2008; 19: 533- 537.
10. Pantvaidya GH, Pramesh CS, Deshpande MS, Jambhekar NA, Sharma S, Deshpane RK. Small cell carcinoma of the esophagus: the Tata Memorial Hospital experience. Ann Yhorac Surg 2002; 74: 1924-7.
11. Yau KK, Siu TW, Wong DC, Chau H, Li CAN, Law BKB, Li MKW. Non-operative management of small cell carcinoma of the esophagus. Dis Esophagus 2007; 20 (6): 487-90.
12. Casas F, Ferrer F, Farrus B, Casals J, Biete A. Primary small cell carcinoma of the esophagus: a review of the literature with emphasis on therapy and prognosis. Cancer 1997; 80: 1366-1372.
13. Brenner B, Shan MA, Gonen M, Klimstra DS, Shia J, Kelsen DP. Small-cell carcinoma of the gastrointestinal tract: a retrospective study of 64 cases. Br J Cancer 2004; 90 (9): 1720 – 6.
14. Huncharek M, Muscat J. Small Cell carcinoma of the esophagus. The Massachussets General Hospital experience, 1987 to 1993. Chest 1995, 107(1): 179-181.
15. Lv J, Linag J, Wang J, Wang L, He J, Xiao Z, Yin W. Primary Small Cell Carcinoma of the Esophagus. J Thorac Oncol. 2008;3: 1460–1465.
16. Medgyesy CD, Wolff RA, Putnam JB Jr, Ajani JA. Small cell carcinoma of the esophagus: the University of Texas M.D. Anderson Cancer Center experience and literature review. Cancer 2000; 88: 262-267.
17. Bennouna J, Bardet E, Deguiral P, Douillard JY. Small cell carcinoma of the esophagus. Analysis of 10 cases and review of the published data. Am J Clin Oncol 2000; 23 (5): 455-459.
18. Ho JK, Herrera GA, Jones JM, Alexander CB. Small cell carcinoma of the esophagus: evidence for a unified histiogenesis. Hum Pathol 1984; 15: 460-8.
19. Nemoto K, Zhao HJ, Goto T, Ogawa Y, Takai Y, Matsushita H, Takeda K, Takahashi C, Saito H, Yamada S. Radiation therapy for limited-stage small cell esophageal cancer. Am J Clin Oncol 2002; 25 (4): 404-407.
20. Lam KY, Law S, Tung P, Wong J. Esophageal cell carcinomas. Clinicopathologic parameters, p53 overexpression, proliferation marker and their impact on pathogenesis. Arch Pathol Lab Med 2000; 124: 228-233.
21. Ho JK, Herrera GA, Jones JM, Alexander CB. Small cell carcinoma of the esophagus: evidence for a unified histiogenesis. Hum Pathol 1984; 15: 460-8.
22. Nemoto K, Zhao HJ, Goto T, Ogawa Y, Takai Y, Matsushita H, Takeda K, Takahashi C, Saito H, Yamada S. Radiation therapy for limited-stage small cell esophageal cancer. Am J Clin Oncol 2002; 25 (4): 404-407.
23. Lam KY, Law S, Tung P, Wong J. Esophageal cell carcinomas. Clinicopathologic parameters, p53 overexpression, proliferation marker and their impact on pathogenesis. Arch Pathol Lab Med 2000; 124: 228-233.
Correspondence Address: Manoop S. Bhutani,MD,FACG,FASGE,FACP,AGAF; Professor of Medicine, Experimental Diagnostic Imaging and Biomedical Engineering; Eminent Scientist of the Year 2008, World Scientist Forum; Director of Endoscopic Research and Development; Department of Gastroenterology, Hepatology and Nutrition-Unit 1466; UT MD Anderson Cancer Center; 1515 Holcombe Blvd., Houston, Texas,USA 77030-4009;Phone:713-794-5073; Fax:713-563-4398; manoop.bhutani@mdanderson.org...”
___________________________________________________
6. https://www.ncbi.nlm.nih.gov/pubmed/10640955
“Format: Abstract - Cancer. 2000 Jan 15;88(2):262-7.
SMALL CELL CARCINOMA OF THE ESOPHAGUS: THE UNIVERSITY OF TEXAS M. D. ANDERSON CANCER CENTER EXPERIENCE AND LITERATURE REVIEW.
Medgyesy CD1, Wolff RA, Putnam JB Jr, Ajani JA. - Author information
Abstract - BACKGROUND:
Small cell carcinoma of the esophagus is a rare disease with aggressive behavior and poor prognosis. Multidrug chemotherapy remains the treatment of choice given the systemic nature of the disease. Radiotherapy has been used concurrently with chemotherapy to enhance local control. The role of surgery in patients with limited disease is controversial. Limited data exist regarding the pathologic response of the tumor to chemoradiotherapy. The goal of the current study was to analyze the outcome of 8 patients treated at the M. D. Anderson Cancer Center, with particular focus on the histologic findings of the resected specimens.
METHODS:
Patient records were reviewed for demographics, presenting symptoms, diagnostic modalities, disease stage, treatment, and outcome.
RESULTS:
Two of eight patients had metastatic disease at the time of diagnosis and received combination chemotherapy.
Six patients had limited stage disease.
Four received combined modality treatment including esophagectomy, and two received radiotherapy only.
All four patients who underwent esophagectomy had pure small cell carcinoma histology at diagnosis and received preoperative combination chemotherapy with or without radiotherapy.
None of the four patients achieved a pathologic complete remission.
Two patients had residual small cell carcinoma; one patient had squamous cell carcinoma and one adenocarcinoma.
The median overall survival for the group of patients was 12.5 months (range, 5-57 months).
CONCLUSIONS:
In selected patients with limited stage disease, surgery with curative intent should be considered as part of multimodality treatment.
Copyright 2000 American Cancer Society…”
___________________________________________________________________
7. https://www.ncbi.nlm.nih.gov/pubmed/9587362
“Format: Abstract - Bull Cancer. 1997 Dec;84(12):1109-14.
[SMALL CELL CARCINOMA OF THE ESOPHAGUS. Report of five cases with review of the literature]. [Article in French] Bennouna J1, Douillard JY, Bardet E, Maury B. Author information –
Abstract
Small-cell carcinomas of the esophagus are a rare and aggressive tumors with early widespread dissemination. Despite the use of different therapeutic modalities, the prognosis remains poor. Between 1993 and 1995, 5 patients with small-cell carcinoma of the esophagus were treated at René-Gauducheau Center, representing 2.8% of all esophageal malignancies diagnosed during this period.
Three patients presented with limited disease while 2 patients had distant metastases at the time of diagnosis. Primary treatment consisted of polychemotherapy in all patients and a complete response was observed in three cases. These 3 patients had received subsequent radiotherapy, and endoesophageal brachytherapy in 2 cases. In this article, we report our experience of patients with this tumor and attempt to make comparisons with the cases published in the literature, regarding location, symptomatology, histopathologic diagnosis and treatment of this tumor. We conclude that the optimum treatment seems to be the same as for small-cell carcinoma of the lung, a multidrug combination chemotherapy regimen used alone or with sequential radiation…”
___________________________________________________________________
8. https://www.ncbi.nlm.nih.gov/pubmed/26734479
“Format: Abstract - Iran Red Crescent Med J. 2015 Nov 1;17(11):e20353. doi: 10.5812/ircmj.20353. eCollection 2015 Nov.
SMALL CELL CARCINOMA OF THE ESOPHAGUS: Clinicopathological Features and Outcome of 22 Cases…”
____________________________________
9. https://www.ncbi.nlm.nih.gov/pubmed/17299393
“Format: Abstract - Br J Cancer. 2007 Mar 12;96(5):708-11. Epub 2007 Feb 13.
SMALL CELL OESOPHAGEAL CARCINOMA: an institutional experience and review of the literature.
Hudson E1, Powell J, Mukherjee S, Crosby TD, Brewster AE, Maughan TS, Bailey H, Lester JF.
Abstract
Primary small cell oesophageal carcinoma (SCOC) is rare, prognosis is poor and there is no established optimum treatment strategy. It shares many clinicopathologic features with small cell carcinoma of the lung; therefore, a similar staging and treatment strategy was adopted…”
___________________________End of references________________________
0
Discussion Boards
- All Discussion Boards
- 6 CSN Information
- 6 Welcome to CSN
- 121.2K Cancer specific
- 2.8K Anal Cancer
- 440 Bladder Cancer
- 306 Bone Cancers
- 1.6K Brain Cancer
- 28.4K Breast Cancer
- 391 Childhood Cancers
- 27.9K Colorectal Cancer
- 4.6K Esophageal Cancer
- 1.2K Gynecological Cancers (other than ovarian and uterine)
- 12.9K Head and Neck Cancer
- 6.3K Kidney Cancer
- 666 Leukemia
- 789 Liver Cancer
- 4.1K Lung Cancer
- 5.1K Lymphoma (Hodgkin and Non-Hodgkin)
- 235 Multiple Myeloma
- 7.1K Ovarian Cancer
- 53 Pancreatic Cancer
- 486 Peritoneal Cancer
- 5.3K Prostate Cancer
- 1.2K Rare and Other Cancers
- 532 Sarcoma
- 717 Skin Cancer
- 647 Stomach Cancer
- 190 Testicular Cancer
- 1.5K Thyroid Cancer
- 5.8K Uterine/Endometrial Cancer
- 6.3K Lifestyle Discussion Boards


 https://www.youtube.com/watch?v=SkQiw271ZT4
https://www.youtube.com/watch?v=SkQiw271ZT4