Dad's early cancer and EMR
Hi!
My dad has diagnosed with early stage esophageal cancer when he had he's endoscopy. He had what is called "inlet patch" in hir upper esophagus and it was causing him pain. it was small, about 1,5cm wide but there were SCC found in it. Anyway, then he had EMR and pathology tests were made again and now there weren't signs of cancer?! They weren't able to get tho whole inlet patch to pathologys test but some of it.
Could it still be cancer? He have endoscopy again next week. This waiting game is nerve wrecking.
Thanks!
- Jimena123
Comments
-
Jimena~Hope info here helps U2 B better informed re Dad's cancer
Good afternoon Jimena,
All who read your letter can identify with your anxious moments waiting to find out just what’s going on with your father’s treatments. You state that he was diagnosed with “early stage cancer.” Not knowing exactly what stage that would be classified as, please see the “Cancer.net” link which will describe the various stages of Esophageal Cancer. As you probably know within the staging system, there is a designation for “T” “N” “M”. Tumor=tumor—N=node—M=metastasis meaning spread.
(TX: The primary tumor cannot be evaluated.
T0: There is no cancer in the esophagus.
Tis: This is called carcinoma (cancer) in situ. Carcinoma in situ is very early cancer. Cancer cells are in only one small area of the top lining of the esophagus without any spread into the lining.)
So be sure to ask the surgeon to explain the classification of your father’s final stage as determined. As for the “inlet patch”, it is sometimes said to be “congenital”, meaning it was there from birth. But by its nature, has some acidic qualities to it. Please read the link about the “inlet patch” to understand more about its origin.
Now you use the abbreviation SCC. Is that referring to Squamous Cell Carcinoma? http://www.news-medical.net/health/What-is-Squamous-Cell-Carcinoma.aspx
“…Skin cancers have a higher incidence than any other type of cancer that continues to rise, despite knowledge and public health campaigns about their prevention. Squamous cell carcinoma is the second most common type of skin cancer, after basal cell carcinoma…”
Are you saying that your dad has actually been diagnosed with Squamous Cell Carcinoma of the Esophagus? If so, they should have provided you with a preliminary diagnosis to begin with before they began the “Endoscopic Mucosal Resection.” This is a procedure where the lesion is “scraped” from the lining of the Esophagus as I understand it. But I have also read that is an EMR is performed, that it will require many subsequent returns for retesting to be certain that no more tumors are detected. And for that reason, many surgeons opt to perform the Esophagectomy to begin with because after an Esophagectomy one doesn’t have to make a “lifetime” schedule to constantly be evaluated.
But both types of Esophageal Cancer are covered in the “Cancer.Net” link.
It will be good if when your Dad is retested that the result will be no sign of cancer. But I might suggest that if there is still residual cancer that Dad might want a 2nd opinion which is always recommended. Sometimes no neo-adjuvant chemo or radiation is required if the cancer is very early. We have a friend here in Virginia Beach that was diagnosed with very early cancer, and did not require any pre-op treatments. That was several years ago, and to this day, he is still cancer free.
However, if this EMR has not resolved your dad’s problem, may I suggest you have a 2nd consultation with a noted Thoracic Surgeon thoroughly versed in the technique of Ivor Lewis Minimally Invasive Esophagectomy. (Commonly called MIE). This is a totally laparoscopic esophagectomy which carries with it less hospitalization time, less recuperative period, less morbidity, etc. Be sure you deal with a hospital that has skilled surgeons and is a “high volume” medical facility that majors in Esophageal Cancer Surgeries. My husband’s surgeon is Dr. James D. Luketich that operates out of the University of Pittsburgh Medical Center (UPMC). It is a teaching hospital, and many surgeons have gone there to learn the procedure and/or upgrade their skills. He pioneered the MIE back in the mid 1990s. So these are my suggestions.
Please understand that I am not a medical person, but am thoroughly familiar with many facets in the life of an Esophageal Cancer patient, since my husband is one. We are now in our 14th year of “rejoicing” because his cancer has not returned, thank GOD!
Incidentally, when I first began to research an “inlet patch”, a term not before familiar to me, I read that it was most often congenital. But the acidic nature of the “patch” could lead to further erosion, and eventually could lead to Barrett’s Esophagus. But we also know that long term, Barrett’s Esophagus can also turn into Esophageal Cancer. So at first I thought perhaps it was simply a problem limited to that “patch” on the surface of the Esophagus. But then you said he was diagnosed with an “early cancer”, so that made me wonder if indeed the patch had become cancerous. According to some info, it can develop into Esophageal cancer sometimes.
So Jimina, the information I have provided below is all that I am qualified to help you with, and I hope it will be beneficial to you in understanding just what Esophageal Cancer is all about. I would add one thought, you are entitled to a copy of all the medical records pertaining to your Dad’s condition “free”, and I would ask for a copy each time he receives any kind of treatment. As to your last question, could the pathology turn out that Dad still has cancer? That possibility does exist. And yes, the wait is indeed “nerve wracking!” We hope everything will show to be negative for cancer when the results are known. That would be the best news you could ever hear! We wish the best for you and your dad.Loretta Marshall
Wife of William Marshall, diagnosed EC Stage III (T3N1M0) Nov. 2002. MIE surgery @ UPMC by Dr. James D. Luketich on May 17, 2003!
___________________________________________________________
1. http://www.cancer.net/cancer-types/esophageal-cancer
“This is Cancer.Net’s Guide to Esophageal Cancer. Use the menu below to choose the Overview/Introduction section to get started. Or, you can choose another section to learn more about a specific question you have. Each guide is reviewed by experts on the Cancer.Net Editorial Board, which is composed of medical, surgical, radiation, gynecologic, and pediatric oncologists, oncology nurses, physician assistants, social workers, and patient advocates…”
__________________________________________________________________
2. http://www.cancer.net/cancer-types/esophageal-cancer/stages
“…The results are combined to determine the stage of cancer for each person. There are 5 stages: stage 0 (zero) and stages I through IV (one through four). The stage provides a common way of describing the cancer, so doctors can work together to plan the best treatments.
Here are more details on each part of the TNM system for esophageal cancer:
Tumor (T)
Using the TNM system, the "T" plus a letter or number (0 to 4) is used to describe the tumor, including whether the cancer has grown into the wall of the esophagus or nearby tissue, and if so, how deep. Some stages are also divided into smaller groups that help describe the tumor in even more detail. Specific tumor stage information is listed below.
TX: The primary tumor cannot be evaluated.
T0: There is no cancer in the esophagus.
Tis: This is called carcinoma (cancer) in situ. Carcinoma in situ is very early cancer. Cancer cells are in only one small area of the top lining of the esophagus without any spread into the lining.
T1: There is a tumor in the lamina propria and the 2 inside layers of the esophagus called the submucosa. Cancer cells have spread into the lining of the esophagus.
T2: The tumor is in the third layer of the esophagus called the muscularis propria. Cancer cells have spread into but not through the muscle wall of the esophagus.
T3: The tumor is in the outer layer of the esophagus called the adventitia. Cancer cells have spread through the entire muscle wall of the esophagus into surrounding tissue.
T4: The tumor has spread outside the esophagus into areas around it. Cancer cells have spread to structures surrounding the esophagus, including the large blood vessel coming from the heart called the aorta, the windpipe, diaphragm, and the pleural lining of the lung…”
__________________________________________________
3.
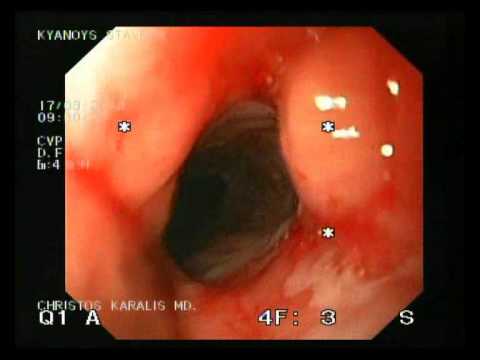 https://www.youtube.com/watch?v=PPnT5rqVqbg
https://www.youtube.com/watch?v=PPnT5rqVqbgHere is a video showing an “inlet patch.”
“ESOPHAGEAL INLET PATCH CHRISTOS KARLIS MD.wmv
"Uploaded on Mar 17, 2010 - Oesophageal cervical inlet patch is considered a congenital anomaly, a remnant of gastric mucosa which is left behind during the descent of the stomach in embryologic development and contains parietal cells that secret acid. Some times even H. Pylori infection can develop in these ectopic gastric mucosa islands. It can be found in about 5% of infants and up to 10% of children. Its presence is estimated at around 8% in adults. Traditionally, Barrett oesophagus is considered a distinct entity from oesophageal inlet patch. Barrett oesophagus is an acquired precancerous lesion and the cell origin probably involves multipotential undifferentiated cells.
Inlet patch is considered to be congenital and has no malignant potential. However, recent studies have challenged these concepts. More and more endoscopic series have demonstrated a frequent association of cervical inlet patch with Barrett oesophagus.
There is a debate regarding to treat or not to treat these patches using EMR or HALO radioablation. If the lesion is associated with Barrett's oesophagus in a symptomatic patient the present tendency is to treat.”
_______________________________________________________________________
4. http://www.mayoclinic.org/tests-procedures/endoscopic-mucosal-resection/basics/what-you-can-expect/prc-20014197
What you can expect - By Mayo Clinic Staff
“There are a few versions of endoscopic mucosal resection. Ask your gastroenterologist about how your procedure will be performed. A common approach includes these steps:
Inserting the endoscope and guiding the tip to the area of concern
-
Injecting a fluid under a lesion to create a cushion between the lesion and healthy tissue underneath it
-
Lifting the lesion, possibly using gentle suction
-
Cutting the lesion to separate it from surrounding healthy tissue
-
Removing the abnormal tissue from your body
-
Marking the area with ink (tattoo) so that it can be found again with future endoscopic exams…”
-
________________________________________________
5. http://www.endoatlas.com/atlas_es.html
This link shows images from the Esophagus
_____________________________________________________
6. http://www.endoatlas.com/es_ge_08.html
This link shows pictures of an “inlet patch” in various forms within the Esophagus. Salmon-colored patch of mucosa found in the proximal esophagus, just below the upper esophageal sphincter. This represents an island of heterotopic gastric mucosa, and appears distinct from the surrounding squamous mucosa, which has a silvery color.
___________________________________________________
7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3554816/
(My note: This is a thorough description of the “inlet patch”. I had never heard of this description before, but I note in the article here that it suggests it may be congenital in nature. See “Introduction” section and please understand that I am not a medical person by trade. I’m not as familiar with this condition as I am other things about Esophageal Cancer. )
“Clinical significance of heterotopic gastric mucosal patch of the proximal esophagus
Abstract -
Heterotopic gastric mucosa of the proximal esophagus (HGMPE), also referred to as “inlet patch” or “cervical inlet patch”, is a salmon colored patch that is usually located just distal to the upper esophageal sphincter.
HGMPE is uncommon with endoscopic studies reporting a prevalence ranging from less than one percent to 18%. Most HGMPE are asymptomatic and are detected incidentally during endoscopy for evaluations of other gastrointestinal complaints. Most consider HGMPE as clinically irrelevant entity. The clinical significance of HGMPE is mainly acid related or neoplastic transformation.
The reported prevalence of laryngopharyngeal reflux symptoms varies from less than 20% to as high as 73.1%. However, most of these symptoms are mild.
Clinically significant acid related complications such as bleeding, ulcerations, structure and fistulization have been reported. Although rare, dysplastic changes and malignancies in association with HGMPE have also been reported. Associations with Barrett’s esophagus have also been reported but the findings so far have been conflicting. There are still many areas that are unknown or not well understood and these include the natural history of HGMPE, risk factors for complications, role of Helicobacter pylori infection and factors associated with malignant transformations. Follow-up may need to be considered for patients with complications of HGMPE and surveillance if biopsies show intestinal metaplasia or dysplastic changes. Despite the overall low incidence of clinically relevant manifestations reported in the literature, HGMPE is a clinically significant entity but further researches are required to better understand its clinical significance.
Keywords: Cervical inlet patch, Laryngopharyngeal reflux, Globus pharyngeus, Neoplasms, Barrett’s esophagus…”
INTRODUCTION
Heterotopic gastric mucosa of the esophagus (HGMPE), also commonly referred to as “inlet patch” or “cervical inlet patch”, is an island of ectopic gastric mucosa that is found in the proximal esophagus[1,2]. Rarely, they can also been found in the other part of the esophagus[2,3]. HGMPE is widely considered to be congenital in nature. However, it has also been proposed to be an acquired condition[1,4,5].
The reported incidence varies from less than one percent[6] to 13.8% in endoscopic studies[7]. Autopsy study has reported higher incidence of up to 70%[1,2].
Commonly reported symptoms include laryngopharyngeal reflux (LPR) symptoms and the prevalence has been reported to be as high as 73.1%[8]. However, most of these symptoms are mild and the management depends on the severity of symptoms. A clinico-pathologic classification has been proposed which categorized HGMPE into five distinct groups based on their clinical, endoscopic and histological characteristics (Table (Table11)[1]. Serious and significant complications of HGMPE have been reported in both adults and the pediatric population[1,2,9]. Interestingly, other common upper aero-digestive disorders have also been linked to HGMPE[2,9]. The clinical significance of HGMPE remains debated due to the limited number of publications. This article reviews the literature and discusses the clinical manifestations and significance of HGMPE in clinical practice…”
___________________End of references__________________
0 -
Discussion Boards
- All Discussion Boards
- 6 CSN Information
- 6 Welcome to CSN
- 121.2K Cancer specific
- 2.8K Anal Cancer
- 440 Bladder Cancer
- 306 Bone Cancers
- 1.6K Brain Cancer
- 28.4K Breast Cancer
- 391 Childhood Cancers
- 27.9K Colorectal Cancer
- 4.6K Esophageal Cancer
- 1.2K Gynecological Cancers (other than ovarian and uterine)
- 12.9K Head and Neck Cancer
- 6.3K Kidney Cancer
- 666 Leukemia
- 789 Liver Cancer
- 4.1K Lung Cancer
- 5.1K Lymphoma (Hodgkin and Non-Hodgkin)
- 235 Multiple Myeloma
- 7.1K Ovarian Cancer
- 53 Pancreatic Cancer
- 486 Peritoneal Cancer
- 5.3K Prostate Cancer
- 1.2K Rare and Other Cancers
- 532 Sarcoma
- 717 Skin Cancer
- 647 Stomach Cancer
- 190 Testicular Cancer
- 1.5K Thyroid Cancer
- 5.8K Uterine/Endometrial Cancer
- 6.3K Lifestyle Discussion Boards
